Medication Allergy Intolerance Contraindication and History of Adverse Reaction
Contents
Welcome to the Medication Allergy, Intolerance, Contraindication, and History of Adverse Reaction roundup circa 2011 page
Prior hashing
http://wiki.hl7.org/index.php?title=Allergy_Intolerance_Model_20070502 http://wiki.hl7.org/index.php?title=Allergy_Intolerance_Model_20070522 http://wiki.hl7.org/index.php?title=Allergy_Intolerance_Models http://wiki.hl7.org/index.php?title=Product_ICSR
Later re-hashing
http://www.hl7.org/v3ballot/html/domains/uvrr/uvrr_SafetyReportManagement.html#PORR_HD049006UV http://wiki.hl7.org/index.php?title=Allergy_%26_Intolerance
Latest discussion
What we really mean
In general, when we talk about "allergies" (in a meaningful use sense) what we really mean is "Don't give these drugs, or expose patients to these substances, without careful thought; and, if you have an ounce of sense, a good reason documented in the chart why you are".
It should be called "Medication and other substances used in a healthcare setting related problems"
What we do now
In any regards, the current LOINC code (48765-2) 'Allergies, adverse reactions, alerts' is where I think we collect these. In looking over the layers of instructions from C32/C83/C80/IHE PCC vol 2/CCD
If you look at the Care provision Health Concern Topic you will see a model that should work. It separates a name for a concern (much like you would link a diagnosis to a problem, rather than equate them, even though at times they are the same concept) and serves to organize related information over time (e.g. episodes of manifestations).
Patient care spent some time about two-three years ago working on harmonizing the various models floating around HL7 to something more or less the same clinical statement pattern. It does depend somewhat on your terminology. This is a great example of where SNOMED-CT is much more useful than other considerations as it has an explicit mechanism to link a disorder with a cause.
What we should do (in the future)
Clinical perspective:
You can have many and different manifestations (e.g. hives, wheezing in the case of true type I hypersensitivity) of the same allergy to a medication, you can also have the same with multiple different allergies to the same medications (e.g. hives and interstitial nephritis in the case type I and type III hypersensitivity).
The allergy list should NOT, ironically, contain lists of what most people who have true allergies are allergic to (mold spores, Ragweed pollen, animal dander, house dust mites, etc.). Go figure.
It really is a set of (usually poorly documented) flags set to fly after (preferably before) you order a medication. Many are safe to ignore, many require additional caution. For example, I used to routinely give a 1/10th dose of oral penicillin to people who had the typical non-specific history of "my mom told me I was allergic" in the emergency department and watch them for an hour or so before letting them go home. It was a slight pain for them, but it did allow them to scratch off an allergy (assuming I didn't kill them).
I got away with this for a very simple reason that many things people refer to as allergies are not allergies. In fact, many are not even anything other than a typical response to a drug that poses little or no threat to the patient, but can really rack up the cost of care, with additional testing, selection of drugs with suboptimal effectiveness, or prescribing more expensive drugs.
This is a case (along with clinically important drug interactions) where having the right information, in the right format, at the right time and place makes a huge difference. This isn't something that can be said across the spectrum of what we do for a living.
Most drug reactions are not allergies, and most allergies are not drug reactions. What we most care about are true allergies (hypersensitivity, e.g. IgE mediated), idiosyncratic reactions which are prone to reoccur (e.g. protracted paralysis after succinylcholine administration due to a congenital deficiency in plasma pseudo-cholinesterase---I think I am fingering the right enzyme here), and some adverse drug reactions which may occur in this particular patient, even though they occur in everyone (e.g. vomiting with codeine, salmon-pink bumpy rash with amoxicillin used to treat a viral infection in childhood).
From a v3 (or v3.1 come May) modeling perspective, it is just another problem. If you are prone to airway closure due to upper airway swelling (angioedema) due to an idiosyncratic (non-allergic, mind you) reaction to ACE inhibitors, or fish does this to you, you have a problem. So it is part of your list of health concerns.
Since these are of particular importance in a healthcare setting, from a patient safety point of view, long ingrained in centuries of pre-Gutenberg patient records, we call these out as special. The third question I ask everyone while they are being whisked from ambulance into my emergency department is "do you have any medications you cannot take or allergies to medications?" (purists will argue this is two questions).
Often it takes us a long time to figure out that a problem is being caused by exposure to a specific medication or other substance (e.g. natural latex). To make this worse, people will have adverse effects of medications which should never be included in their "allergies" list.
For instance, hypokalemia with furosemide, somnolence with zolipidem, bradycardia with propranolol all sound worrisome, which them can be (if extreme). However, since these are the actual effects the drugs do, and are only a problem in certain circumstances (e.g. you didn't prescribe enough potassium supplement with furosemide, or are giving propranolol in too high a dose or to someone with renal impairment).
If someone, however, is particularly sensitive/insensitive to effects of a particular drug (most often a class of drugs) then it may be worth adding an entry under "allergies", but with the caveat that every time someone tries to prescribe the RIGHT dose (unless someone has come up with a really advanced system and forgot to tell me about it) they will get the same alert as someone trying to give them the wrong dose.
The day we include pharmacogenomic and drug metabolism genetic testing to the new born screen will both be a mess, as well as a most welcome a blessing. So keep this in mind when building systems. You may end up with "allergies" to something the patient may never, ever take or need.
So, this, like most of medicine, is complex and our traditional approach (i.e. allergies list, problem list) just don't really capture the essence that we can with electronic systems.
Sorting out of codes
Complete with unambiguous definitions
Codes used in DEEDS
Allergies, adverse reactions and alerts (LOINC 48765-2) History of adverse drug reaction (LOINC 44939-7) Reported Medication Allergy (LOINC 11382-9)
Old and new templateIds
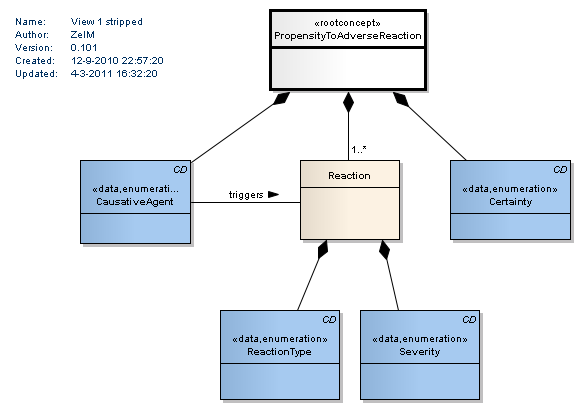
Propensity to Adverse Reaction DCM
This is what we came up with. This DCM was the result of "merging and trimming" the HL7 model, CCD and CUI ADR guidance. Note that we use this for registration of the propensity. After that there are views to register Adverse Events and to register the Test Results. CTCAE is not usable as severity since that is about an Adverse Event, not about the propensity.