Da Vinci Prior Authorization FHIR IG Proposal
Da Vinci Prior Authorization FHIR Implementation Guide
Contents
- 1 Owning work group name
- 2 Committee Approval Date:
- 3 Contributing or Reviewing Work Groups
- 4 FHIR Development Project Insight ID
- 5 Scope of coverage
- 6 IG Purpose
- 7 Content location
- 8 Proposed IG realm and code
- 9 Maintenance Plan
- 10 Short Description
- 11 Long Description
- 12 Involved parties
- 13 Expected implementations
- 14 Content sources
- 15 Example Scenarios
- 16 IG Relationships
- 17 Timelines
- 18 When IG Proposal Is Complete
- 19 FMG Notes
Owning work group name
Financial Management
Committee Approval Date:
- 1/16/2019, approved the original HL7 #1490 PSS to produce an IG for FHIR. Approved on 2/19/2019
Contributing or Reviewing Work Groups
- Attachments
FHIR Development Project Insight ID
- 1490
Scope of coverage
The scope of this implementation guide is:
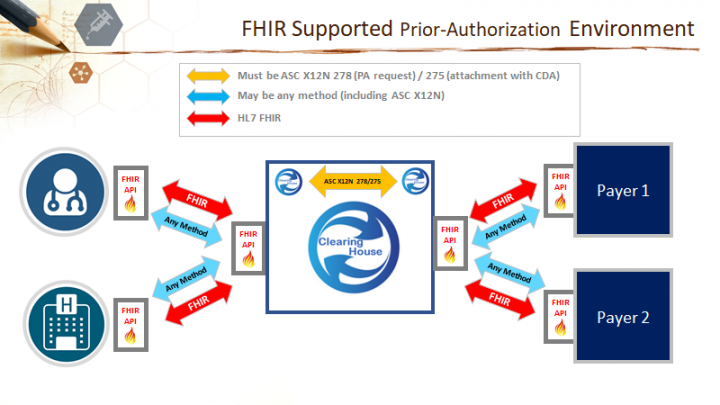
- A FHIR-based B2B process to allow implementers to use existing IT infrastructure resources for exchanging prior authorization. Existing business agreements can also be reused.
- The goal is to define FHIR based services to enable provider, at point of service, to request authorization (including all necessary clinical information to support the request) and receive immediate authorization.
- The assumption is that this use case will leverage the ASC X12N 278 and 275 for compliance with HIPAA.
- Clearinghouses can continue to route and translate data as appropriate.
- The project will investigate the ability to enable a translation layer to convert FHIR resources to HIPAA format and from HIPAA format back to FHIR.
This PSS builds on existing or in process implementation guides for the automation of coverage discovery (Coverage Requirements Discovery – CRD), definition of documentation and payer rules (Documentation Templates and Payer Rules) access to provider information (Clinical Data Exchange – CDex) and the Health Record Framework (HRex).
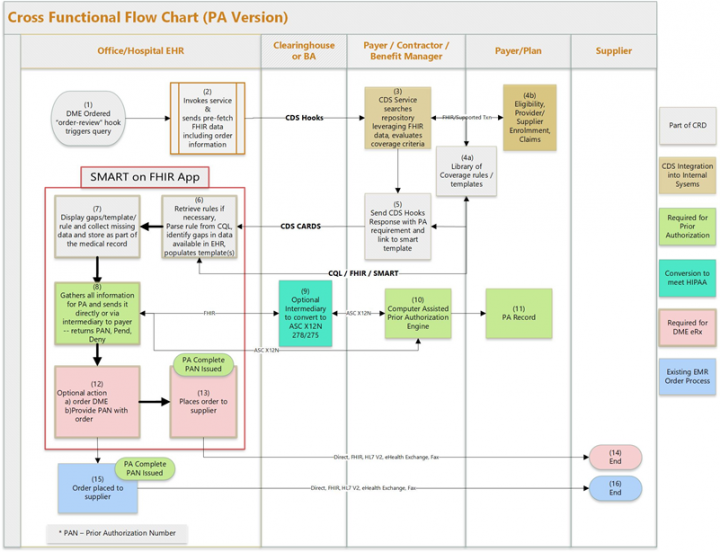
This project will define specific triggers and exchange methods (CDS Hooks, Push, etc.), use of other interoperability "standards" (e.g. SMART on FHIR, CQL) and specific use of FHIR resources to effectively exchange payer information regarding the services that need authorization for coverage.
The following diagrams depicts the flow and scope of the relevant information (they are illustrative and not fully prescriptive).

This project will reference, where possible the "standards" defined by the Health Record exchange (HRex) Framework Implementation Guide which in turn will utilize prior work from Argonaut, US Core and QI Core effort for FHIR DSTU2, STU3, and R4. The following diagram depicts the anticipated scope of the HRex Framework IG.
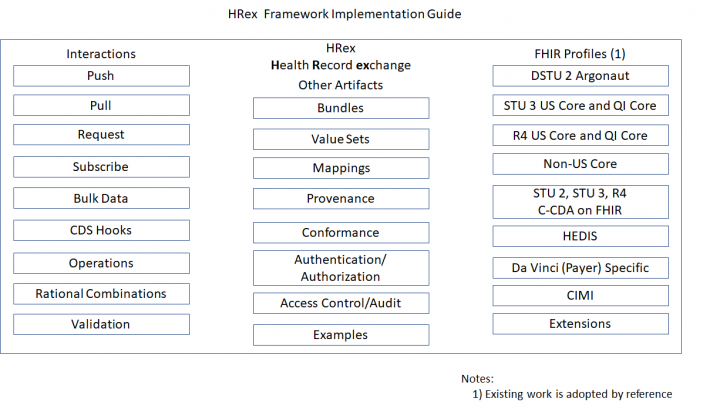
The ultimate goal is to support the request, collection of existing information, solicitation of addition information (where required), packaging and exchange of provider information on a specific patient for satisfy the requirements for payer authorization for specific services using technology that supports FHIR DSTU2, STU3, and R4 releases of the FHIR standard.
The project team plans to work with existing FHIR artifacts where possible. If changes are necessary, the project team will work with the responsible Work Group to review and implement (via tracker items or new PSS) any necessary enhancements to base FHIR resources, extensions, and/or profiles.
This project will not include mapping to X12 standards and code sets (unless approved by joint agreement between HL7 and X12) – but this step is essential to the end-to-end workflow
IG Purpose
Providers need the ability, in clinical workflow, to easily identify the need for payer authorizations, assemble necessary information, identify and supply missing information and submit it to the payer electronically. Payers should be able to respond to a number of requests for authorization in "real time" to allow the provider to move forward with treatment as soon as possible. This PSS builds on existing or in process implementation guides for the automation of coverage discovery (Coverage Requirements Discovery – CRD), definition of documentation and payer rules (Documentation Templates and Payer Rules) access to provider information (Clinical Data Exchange – CDex) and the Health Record Framework (HRex). Currently, no FHIR implementation guide exists to standardize the method of requesting, validating, soliciting, packaging and exchanging (request, response) information required for payer authorizations. This implementation guide will provide a standard for adoption by both providers and payers for the exchange of information necessary for authorization of services by a payer.
Content location
https://github.com/HL7/priorauth
Proposed IG realm and code
US/Davinci-PriorAuth
Maintenance Plan
The Da Vinci Project has committed to maintaining the guides, in conjunction with the responsible workinggroup, for the next 4-5 years. (it was just confirmed on the 2/6/2019 Operating Committee Meeting.)
Short Description
Providers need the ability to easily identify the need for payer authorizations, assemble necessary information, identify and supply missing information and submit it to the payer electronically and receive a response in "real time" within the clinical workflow.
Long Description
Providers need the ability, in clinical workflow, to easily identify the need for payer authorizations, assemble necessary information, identify and supply missing information and submit it to the payer electronically. Payers should be able to respond to a number of requests for authorization in "real time" to allow the provider to move forward with treatment as soon as possible. This PSS builds on existing or in process implementation guides for the automation of coverage discovery (Coverage Requirements Discovery – CRD), definition of documentation and payer rules (Documentation Templates and Payer Rules) access to provider information (Clinical Data Exchange – CDex) and the Health Record Framework (HRex). Currently, no FHIR implementation guide exists to standardize the method of requesting, validating, soliciting, packaging and exchanging (request, response) information required for payer authorizations. This implementation guide will provide a standard for adoption by both providers and payers for the exchange of information necessary for authorization of services by a payer.
Involved parties
- Financial Management Work Group
- Da Vinci Project
This implementation guide will be developed by Financial Workgroup as part of the Da Vinci project.
Expected implementations
- Cerner
- Cambia
Content sources
Da Vinci use case development, FM/Da Vinci working group calls related to Prior-Authorization Support, and other Da Vinci / Workgroup calls with relevant content for this IG (e.g. CRD, DTR, HRex, CDex)
Example Scenarios
- PCP wants to refer patient to specialty care. Requires an authorization from the Payer.
- Patient to be discharged to home, but needs full time oxygen therapy. This requires an authorization, but which DME provider is the preferred provider for the home address, is there any additional documentation needed?
IG Relationships
Utilizes the CRD IG to trigger the interaction with the payer
This project will reference, where possible the "standards" defined by the Health Record exchange (HRex) Framework Implementation Guide which in turn will utilize prior work from Argonaut, US Core and QI Core effort for FHIR DSTU2, STU3, and R4.
Timelines
Submit for STU Ballot
2019 May Ballot
When IG Proposal Is Complete
When you have completed your proposal, please send an email to FMGcontact@HL7.org 2019 Sep Ballot?