May 2014 WGM Phoenix: May 4 to May 9
- Back to Patient Care
- Back to 2014 PCWG WGM Agenda and Minutes
Phoenix WGM - May 2014 Patient Care WG Meeting draft agenda:
Contents
Phoenix WGM - May 2004. Patient Care WG Meeting Meeting Minutes
Patient Care WGM, Monday, May 5, 2014
- Back to Patient Care
- Back to 2014 PCWG WGM Agenda and Minutes
Patient Care Monday Q1
Present:
• Stephen Chu (chair)
• Michael Tan ( Scribe)
• Elaine Ayres
• William Goossen
• Iona Thraen
• Christina Knotts
• Cathy Rice
• Jay Lyle
• Russel Leftwich
• Kevin Coonan
Minutes:
Agenda:
• Approval of minutes of San Antonio
• Agenda for the week - Phoenix WGM
• Review PCWG 3 year plan
• Any other business
Minutes of San Antonio:
• San Antonio WGM draft minutes available on Patient Care WG wiki within 48 hours post WGM
• There were no discussions.
• Elaine moved to approve the minutes, Russ second.
• Vote: 8 approved, 0 abstain, 0 agains.
• San Antonio WGM minutes approved as official record of the WGM
Agenda for the week:
• Need some time for new proposals:
- New FHIR Clinical Document PSS discussion
• The agenda reviewed and spreadsheet is updated with scribe/ chair.
• Their is an interest for a joint project but Anesthesia does not have the bandwidth to carry out the work and relies on PCWG to do the work. Issue is whether we should carry on.
- Need to discuss with Anesthesia WG re whether PCWG needs to dedicate a quarter for joint meeting
• Arrangement had been made for Tuesday lunch quarter meeting with FHIR
- Agenda - to discuss clinical inputs to FHIR resources development and review
- Need enough resources for the joint lunch with FHIR ( Hopi).
• Need to replan the September WGM with CQI.
3 year work plan:
o PCWG did not get their gold award, because we did not submit the ballot for Allergies.
o The project list has been cleaned up.
New PSS for Allergy terminology will be submitted. This is a joint with IHTSDO.
A new PSS for Care Plan Clinical Models will be submitted.
The remaining projects were reviewed. Project 927 and 668 are about Vital Signs, but the material on the projects could not be found. It did not go into the DESD. 668 did have a RMIM that according to William could still be used.
881 on the allergies is informative. Does a DAM go into normative? It has already been published.
The project list is a list of active projects.
Motion to remove projects 881 and 745:
- Elaine moved the motion, second by William.
- Vote: 8 approve, 0 abstain, 0 against
Also 664 ( assesment scales) to be removed.
661 (DAM Medical Device). A lot of good work has been done, but Sigoureay is no longer active and the VA is not sponsoring the project anymore. This was balloted in 661, but the ballot spreadsheet could not be found. William wants to keep this on the list, and will look for the ballot material in january 2015. (after September).
320 is about DCM and this needs to be reballoted. This is not worth while.
Elaines moves to close project 664 and 320. Second by William:
- Vote: 8 approve, 0 abstain, 0 against.
Question whether a PSS should be set up for FHIR profiles for extensions. The FHIR resource will only cover 80% of the use cases. The 20% would fall into extensions, that would have to worked out in these profiles. This will be deferred.
Patient Care Monday Q2
PCWG hosting CQI with representative from Clinical Genomics
Present:
Stephen Chu – Chair
Elaine Ayres – Scribe
Michael Tan
Enrique Menses
Patty Craig
Christina Knotts
Thomson Kuhn
Floyd Eisenberg
Rosemary Kennedy
Mollie Cullere
Kimberly Smuk
Kendra Hanley
Ken Rubin
Stan Rankins
Christopher Millet
Walter Suarez
Crystal Kallem
Russell Leftwich
Marc Hadley
Kanwarpreet Sethi
Evelyn Gallego
Best West
Kevin Coonan
Minutes:
Goal of Meeting: Look at CQI projects related to clinical outcomes. PC interested on how PC artifacts can support CQI initiatives.
CQI group presenting current project/measures as well as proposed new measures.
1. VTE-4 (Venous Thromboembolism) – relates to the Care Plan. Are there specific discharged instructions in the care plan and were they followed? QADM/QRDA not yet fully supporting. Need to know where the Care Plan instructions are captured, as well as how they are conveyed. Finding some plans are created by conditions. Instructions may span a variety of orders.
- - QDM/HQMF representation, vs the QRDA – still not harmonized.
- - Family history elements /genomics – looked at the family pedigree model vs. the family history in the Care Plan DAM.
- - Looking at the Care Plan DAM vs. the CDA Care Plan – aligned at this point.
- The Care Plan – identifies a health concern with resulting goals and monitoring.
- The issue of an order is not addressed in the Care Plan DAM – that depends on the implementation, such as through Physician or Nurse order entry applications
- - An order however may be captured as the instructions to the patient, but the order execution and completion is not.
- Did the individual receive the instructions, vs. the outcomes of having received the intructions.
- - To meet the goals in the care plan – results reside in the EHR.
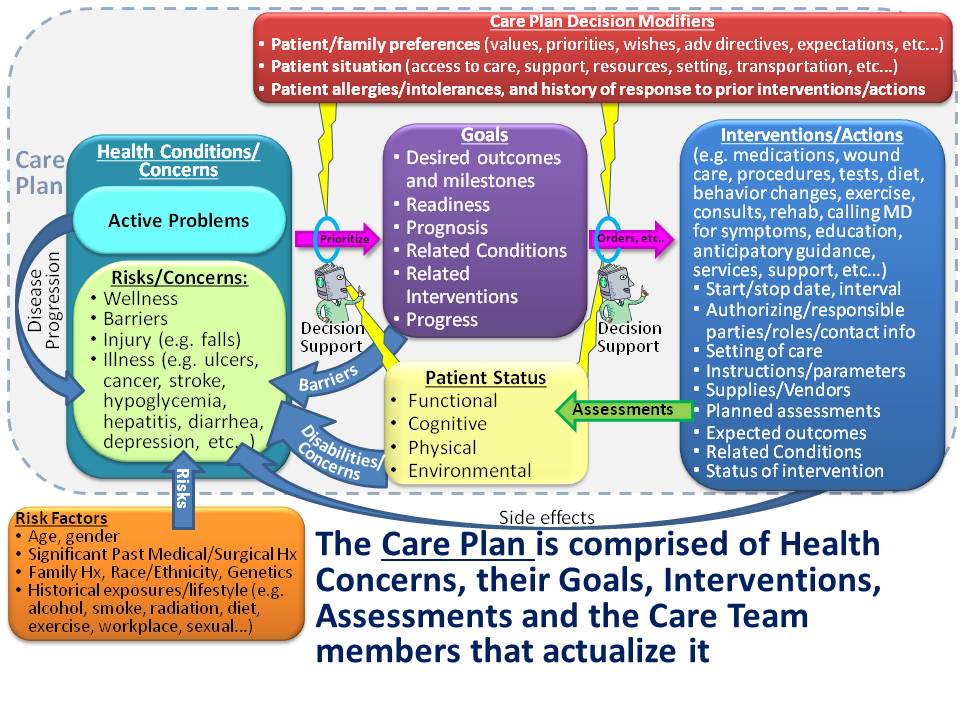
- Patient Care (Russ) displayed the Care Plan model overview slide. Note active problems with risks and concerns, goals and interventions/actions.
- As a care plan is updated, how do you ensure that a quality measure is updated appropriately. Must consider both quality measures as well as CDS.
- With a goal – did you meet the goal?
- CMS will be looking for specific elements, and changing care planning may create a misalignment (e.g. dynamic care plans).
2. Measure Gaps Care Coordination
- a. Where might measurements be done that don’t currently exist? A recent call for new measures did not result in any new measures.
- b. Example – transfer a care plan to the next venue of care, is there a roster (list) of care team members and family members, are care barriers captured in the care plan, are interventions linked to each goal, is there progress towards the goal, is acceptance of the goals by the patient captured, has the care plan been sent to the patient/family or electronic access, is the care plan sent to active care team members in other organizations.
- - Note that there is the Care Plan DAM as well as the Care Plan Services (CCS) and the C-CDA Care Plan document.
- Enrique presented the Care Plan RMIM. Each care plan entry has actors, activities (orders, interventions, instructions, education for example), care barriers, risk (more health risk), patient preferences, goal review and plan review. These all fit into the health concern pattern.
- Examples of barriers – functional limitation, language, financial.
- Risks – can also be dynamically represented.
- There is no specific follow-up for assessment progress toward goals in the care plan model. In the care plan there is a plan review (in total) and goal review and milestones. Is that sufficient to meet that requirement?
- There is no “order” to do the follow-up, but there is a review step. Can also plan the next review. Currently there are no functional requirements but the next review is specified with day/time. Can also distinguish a planned review vs. a completed review.
- Have not stipulated who might review the care plan. There is also an acceptance review (by the patient) and the outcomes review.
- Chicago WG meeting – September – Wednesday Q2 offered as an alternative. Confirmed that day and quarter for the upcoming WG meeting.
Patient Care Monday Lunch Quarter
Allergy/Intolerance and Adverse Reaction Project: Terminology project meeting
Present:
Minutes:
- Slide deck presented at meeting:
Patient Care Monday Q3
Present:
• Stephen Chu (chair)
• Michael Tan ( Scribe)
• Elaine Ayres
• Iona Thraen
• Evely Gallego
• Farrah Darbouze
• Angelique Cortez
• Katherine Duteau
• Jim McClay
• Laura Heermann
• Christina Knotts
• Russel Leftwich
• Kevin Coonan
Minutes:
Topic of the session is on Health Concerns:
• the last model was constructed after the conference call of 17th April. Stephen explains the mind map. This has been agreed but Michael has problem with word event. Event implies a one time happening, while a concern could be chronic. This word was suggested by Larry.
• Iona questions about genetics related concerns. These genetics risc which will be put in family history. It is not the concern itself. Suggest to put it in the model, because this topic is a hot topic. The bucket for risks is bottomless. The picture will be adapted with dots.
• Suggestion from Kevin to tease the risks out and risk observation. This suggestion was not supported.
• The health concern event is the activity to document the health concern.
• Evelyn asks how health concern relates to problem list? A health concern has a technical and a clinical concept. The clinical concept has been defined in San Antonio in the wiki.
• A problem list is a contextual dependent translation of the health concern.
• Some discussion arises about the difference of health concern from care plan and from health concern.
• Are health concern and health concern event 2 separate classes? According to Laura this is where the exacerbation comes in.
• Suggestion from Laura to readdress the picture so that the focus is not so much on the event, but more on the health concern itself or put the health concern as a title.
• It has been decided to replace the word "trigger with the word "contains". Action Stephen.
- - Action completed. Revised "Health Concern" conceptual model uploaded to Health Concern project wikil
• Kevin volunteers to make the logical models. This should be UML diagrams.
• Kevin brings in a motion to make a DAM with only mind maps instead of UML's.
• Iona places a friendly amendment to do both ( Mindmap and UML). Elaine seconds the amended motion:
- - Vote : 1 abstain,1 against, 10 approve.
Patient Care Monday Q4
Present:
Stephen Chu (Chair + Scribe)
Laura Heermann Langford
Enrique Meneses
Iona Thraen
Michael Tan
Christina Knotts
Evelyn Gallego
Kevin Coonan
Minutes:
Care Plan DAM Project update and ballot reconciliation meeting
- Stephen provided an update of Care Plan DAM second informative ballot package development leading to May 2014 ballot package submission.
- Overview of ballot statistics:
- 54 (affirmative) 7 (negative) 56 (abstain) 24 (no vote)
- Quorum: 82.98%
- Overview of ballot spreadsheet was done
- Ballot comment disposition began
- details - see disposition decision and comments in aggregated spreadsheet
Patient Care Monday Q5:
Patient Care co-chairs attended co-chairs dinner meeting and DESD meeting
No PCWG specific meeting held for Monday Q5
Patient Care WGM, Tuesday, May 6, 2014
- Back to Patient Care
- Back to 2014 PCWG WGM Agenda and Minutes
Patient Care Tuesday Q1
Care Plan DAM ballot reconciliation - total comments: approx 100.
Present:
Laura Heermann-Langford – Chair
Elaine Ayres – Scribe
Enrique Menses
Iona Threan
Kevin Coonan
Lenel James
Russ Leftwich
Minutes:
- Lines #5 – remove author names – Persuasive
- Line #6 – wording is excessive re payors and care planning. Rewrite to be more consistent with other storyboards. – Persuasive with mmod.
- Line #7, 8, 9- Storyboards with actors – actor names are too long and confusing in the text. Persuasive with mod – will make shorter actor names. Laura will submit names to names registry.
- Line #10 – Description of Health Plan Disease Management Nurse Care Manager Encounter – a complex use case with multiple actors, care crossing state lines, roles between payors and providers. Note that this is a universal document, not US realm only. Note that Figure 5 – Organizing Framework for Coordination of Care Interaction Models notes that Business Role or Policy is out of scope… comments are persuasive with mod. Simplify the use case, making it more clear who is doing what when. Look at diagramming the the CaseMan/DiseaseMan case using the diagram in the CCS ballot document.
- Line #11 Encounter G – missing content. Comment is persuasive to add missing content.
- Line #12 – Appendix of the storyboard – landed in the middle of the document on page 56. If the drug content is in the text, the appendix can be removed.
- Line #13 – Appendix issue – determine if even needed. Persuasive with mod.
- - VOTE on Block – Move to block vote: Motion: Lenel Abstain – O, Object – 0, Approve – 6
- Line #63 - Line 1605- 1610 – Comment re inclusion of author who is not an HL7 member. Will remove non-member care. Persuasive with mod.
- Line #64 – not best care practice. Persuasive with mod to rewrite.
- - VOTE on Block – Move to block vote: Motion: Lenel Abstain – O, Object – 0, Approve – 6
- Line #65 – insufficient info to describe condition – Persuasive with mod. Will add additional information. Note that a CDA can be used to share information, but not the only means for sharing. Discussion of Note # 3 - line 1660 (Page 46) – discussion of the various types of technology to drive information exchange. Continue to discuss this issue.
- There are several more comments related to Storyboard 8.
Patient Care Tuesday Q2
Patient Care hosting Anaethesiology
Present:
Elaine Ayers (Chair)
John Walsh
Terri Monk
Russell Leftwich
William Goossen
Andrew Norton
Martin Hurrell
Farrah Darbouze
Michael Tan
Stephen Chu
Minutes:
- History
- - Detailed Clinical Model – started at Intermountain Healthcare with Clinical Element Models (5000). IHC do not have a binding to Loinc or Snomed, experts in clinical modeling in Brisbane came together in Hl7, problem with Computational explosion (2005-2007). Find different way of representing in HL7 without breaking HL7 messaging. Implementation issues associated with implementation.
- - Can we have a registry to manage risk? What about patient safety issues? ISO would start on a standard for DCM using top ten, ie vitals, Bartel, Braden, Apgar scores. HL7 created a project #320.
- - HL7 has asked to have work reballotted – where does the work need to be done – CDA, FHIR, SDC, S & I Clinical element repository. Recognition that clinical data element need to be standardized.
- - NLM has protype that is being tested using CDE for clinical research and Patient Safety with AHRQ.
- - The CDE repository approach using a federated approach, SDC would define syntact of the data elements, CMS would publish the algorithm of how the elements come together. All the CDE are using the same structure, would set up federated approach for finding a common data element. S & I defining the syntact of CDE. If sending out must map to the S & I structure for orders and observations.
- - Need common ontology to form foundation. Least imperfect approach. Need name, definition, data type, expression, The axis of the domains should follow the ontology.
- - ONC – is developing a registry for clinical research and patient safety reporting. Multiple driving factors fir DCM. CSRA – Cancer Registry for US as a beginning state. Multiple terminologies CADSR
- Collaboration and joint work
- - Done work to define subset of SNOMED terms need coding, Modeling anesthesia record. Need to take abstract model and translate into CDA. Some of the modeling may actually be a DCM that would need review.
- - Need UML representation of DCM – BP as example. Need to specify the complexities associated with with the measure.
- - HL7 and ISO spec matches 99% except for unclarities from clinical vs implementation. What is the methodology – collection use cases, start there, go to literature, basic text books, clinical common sense and knowledge behind it.
- - Use cases exist. Take original work and update or take ISO work. Unless William takes on work Patient Care work group doesn’t have band width. HL7 wants heart rate re-balloted. Heart rate expression in FHIR into UML, XML, FHIR, etc
- - Need generic information model which is expressed differently by individual technically. Every data element gets own UML class.
- - Anesthesiology would provide a piece of what we are doing, could you look at it to see how DCM would look at it and give feedback –
- - Need a project scope document with Anesthesiology as lead, and then submitted to Patient Care Plan Work group. Would allow William to function as content expert. ONC is part of source material and other repositories. Use ISO format to represent it as DCM (ISO TS 13792)
- - Outcome of UML into XML – several examples with some proper XML missing for CDA or HL7 messaging.
- - Example, ie catheter as device, insertion point, where headed, prep before, etc. ending in a very complex model. Properties become quite complex. Part of it is covered by health concerns and allergies but should not be mixed. Start with basics and then build model with components. Template initiative are bounded pretty simply, there are subtleties concerning their relationships in a dynamic manner.
- - User community of this work would be? Particular vendor would reflect the proprietary ownership. No standard agreement on what should be considered. Each site does own thing.
- - Are there common elements that can be exchanged across entities, significant adverse events, allergic reacdtions, need to look at the depth, continuity of care for patient care, quality of care,.
- - The CDA project provides the structure – adding layers
- - Examples of composition, APGAR and time, Development of birth development, Anethesiology does not know how it can be used until it is accessible.
- What are the next step:
- - Formalized Project Scope Statement or reuse Anesthesiology for this purpose. Already included but is old and needs refreshing. Matters discussed are already in scope as discussed. Update, discuss and get ready for ballot by Jan 2015.
- - Is there a prioritized shopping list for dcms? have candidates and can rapidly prioritized. Current target is produce CDA implementation guide. Tried and tested methodologies could accelerate process by using an example.
- Methods
- - Start with DAM, creates story board, conceptual model and then logical model then put out for two cycles, then map logic model to CCD. Or start with subject matter expertise and then extract a use case from the knowledge as a way of demonstrating that the issues have been well considered. Need to determine if the use case has not broken the model.
- - There is not a need for a DAM for vitals, can pull them in without doing a full process two DCMs are ready, only need an excuse to translate them. Data element from the various repositories needs to be brought in.
- - Anesthesiology will talk about this in their next meeting and get back to Patient Care Work Group.
- - How will DCM will be included in the CDA implementation.
- - Please communicate with chairs.
- William and co-chair will go to Anesthesiology. Joint meeting (Tuesday Q2) in Chicago will be cancelled.
- Slide deck presented at this meeting:
Patient Care Tuesday Lunch Quarter
FHIR: Clinical engagement/inputs into FHIR resources development processes and Clinical connectathon
Present:
Stephen Chu (Chair)
Elaine Ayres (Scribe)
Laura Heermann-Langford
Michael Tan
Russell Leftwich
Jim McClay
Margaret Dittloff
Sandra Marr
Cathy Walsh
Lindsey Hoggle
Kevin Coonan
Lloyd McKenzie
Graham Grieve
David Rowed
Minutes:
- Patient Care Core Resources
- - Should enable best practices Need to support a wide range of implementations.
- - Can ballot profiles as part of the FHIR specification.
- - Have the same type of approach to value sets.
- - What should be in the core – vs as an extension or a profile.
- Question on clinical inputs
- - With existing vendors – you do things because people buy them. Vs. best practice.
- - So, is there core clinical content, that should drive resources. What is current clinical practice?
- - Clinician input – what functionality will help be practice medicine better…
- - FHIR is a platform where you can add new content without breaking the current process. In the CDA spec new info cannot be communicated. With FHIR can add new content (may not be recognized by a receiver…) but it can be sent.
- - To move narrative text only, not an issue. For more function need more structure.
- - Model driven work vs. FHIR model
- - Problem/diagnosis vs. condition.
- Clinical Connectathon – the technical specs are set, but need a review by the clinical community. Would allow users to access data, input and exchange. What is the representation of the data by various clinicians.
- - Use two or three clinical scenarios. Clinicians will enter clinical records, then compare the outcomes of entry. Look at transitions of care.
- - Stephen will organize the collection of use cases that will test processes. (Stephen has sent out an invitation email and will start the organisation process)
- - Will need a size and scope of the connectathon. Have a general scenario and an ED scenario, with an ancillary case.
- - Question – test the questionnaire resource.
Patient Care Tuesday Q3
Care Coordination Services Functional Model updates and ballot reconciliation
Present:
Stephen Chu (Chair)
Iona Thraen (Scribe)
Brian Scheller
Enrique Meneses
Ken Chen
Michael Tan
Mike Grossman
Elaine Ayers
Kevin Cook
Kevin Coonan
Minutes:
- Stephen Chu gave overview
- - progress since first CCS ballot
- - changes to CCS contents leading to May 2014 ballot contents
- CCS ballot overview:
- - Total comments (84) spreadsheet is presented for reconciliation
- Start with the comments that the submitters are in the Tuesday Q3 meeting.
- Negatives maj/min (Brian/Mike)
- - p.26 accept as persuasive: remove constraint 7 0 0
- - p. 27 Global: Persuasive with mod: change person as Patient, Person as provider and other similar classes 7 0 0
- - p.31 Persuasive with modification: change recall to cancel 7 0 0
- - p. Global: Persuasive with Mod: Provide references of sections in DAM to relevant components 7 0 0
- - line 1085: Persuasive with mod: change statement to align with the DAM 7 0 0
- - 1105: Persuasive with mod: change all input to indicate zero or more and add constraint to express existence of at least a health goal
- - Block vote result: 7 (in favour); 0 (abstain); 0 (against)
- A-T
- - Accept all as persuasive
- - Block vote result: 8 (in favour); 0 (abstain); 0 (against)
- A-S
- - Suggestion to add patient consent
- - Persuasive with mod: add functional capability to support patient consent for third party participation
- - Vote result: 8 (in favour); 0 (abstain); 0 (against)
- Ballot reconciliation to continue (next PCWG/SOA joint meeting and conference calls)
Patient Care Tuesday Q4
PCWG hosting FHIR
Present:
Stephen Chu – Chair
Elaine Ayres – Scribe
Lloyd McKenzie
Russ Leftwich
Enrique Meneses
Evelyn Gallego
Farrah Darbouze
Margaret Dittloff
Michael Tan
Jim McClay
Sean Moore
Atanu Sen
Vuay Shah
Iona Thraen
Shreya Soni
Derek White
Laura Heermann Langford
Larry McKnight
Minutes:
- Structured Data Capture PSS
- - This is an S & I Framework project. Primary sponsor is O & O. OO is a co-sponsor. Patient Care is asked to co-sponsor.
- - Project will focus on CDE based on time constraints.
- - Project will create SDC profiles to represent data sets such as VS, allergies, etc. Develop data sets to be used across patient care and research.
- - Goal – to develop a profile that will represent data sets such as vital signs, lab results, medication, problems and allergies. This will enable data sets and common data elements existing within data sets to defined once and reused across health care domains including non-clinical. Define a common syntax based on ISO/EC 1117903 to allow unambiguous interpretations of CDE’s. Will be available in the Observation Definition resource (new).
- - Note that all resources must be international in scope. Goal is for the project – Syntactical harmonization among federal agencies and research communities.
- - Note – planning five profiles. Note cross-over to multiple other projects – FHIM, OpenEHR, templates, CIMI. Is the ISO spec the correct standard – yes, the analysis was completed.
- - Patient Care is asked to ensure the clinical content is appropriate for stated purposes.
- - Vote to approve SDC PSS - Russ/Michael Abstain – 2, Oppose – 0, Affirmative – 14
- FMG Expectations for FHIR Resources – Lloyd McKenzie
- - FHIR DSTU Monitoring – development for next DSTU and supporting implementers for current DSTU. Implementers can request changes on the actual page, in G-FORGE , or on FHIR list-serv.
- - PC WG needs to monitor our assigned resources for questions, concerns etc.
- - We need to assign PC WG to monitor. Need a new PSS for existing resources for maintenance. Want all resources revised to meet quality criteria, profiles for C-CDA, created profiles coming in through the trackers. SEE FHIR Ballot Prep. End goal is next DSTU ballot in January.
- - Also looking at resource proposals and profile proposals on the wiki. There is a check-sheet for QA criteria. Want contexts with examples. An example should use all of the data elements in the resource. Use of extensions – need to be formally defined or give a URL. Don’t use a fake one for example purposes. Look at RIM mappings and verify that they are correct.
- - Value sets – draw on international code systems or national code systems. Don’t invent FHIR specific value sets. Need to be good enough to use in a production system. All codes need proper definitions. If a code is the data type, make sure it is structural. Don’t bind to commercial codes.
- - Data elements – one resource that references another – use the reference in the secondary, not the primary (not both). See if a data element changes another, e.g. status. Identify elements that are summary.
- - Look for consistency across FHIR resources that are similar. Use consistent names when they work. Look for consistency for sort order – critical data elements at the top. Bigger and bulkier data elements at the bottom.
- - Definitions – resolve the to do’s. Provide a rationale for a definition. Target explanation for someone writing code. Capture comments and discussions about adjustments.
- - Manage constraints or make them conditional. Add good descriptions for search criteria.
- - Looking a G-Forge = questionnaire has lots of issues.
- - Patient Care has a band-width issue. Question how we can maintain and develop…..
- - Familiarity with FHIT tools is an issue.
Patient Care Tuesday Q5
PCWG hosting CHWG
Present:
Russ Leftwich – Chair
Elaine Ayres – Scribe
Stephen Chu
Iona Thraen
Enrique Menses
Lindsey Hoggle
Cathy Welsh
Lenel James
Jim McClay
Laura Heermann-Langford
Mike Padula
Cathy Rice
Kevin Coonan
Michael Rossman
Pele Yu
Minutes:
- Discussion of a Portable Health Record for Patients with Complex Health Needs
- - Goal – to help with transitions of care for at risk populations – a prospective care plan for “away from home”.
- Current form includes names health care providers, dx, meds, allergies, procedures, immunizations, problems and findings with management. There are several other flavors as well.
- Initially group was going to make a C-CDA, including elements for the plan of care. However, developing a domain analysis model would be a helpful first step.
- PSS has approved for a DAM – co-sponsors with EC, PC and CBCC. A DAM is useful when requirements are not well established. Key concept is not necessarily the data, rather the management of the individual. This form actually has a care plan embedded in it.
- Should this be a new use case in the Care Plan DAM – and then do a gap analysis and aligned with C-CDA was proposed. Versus developing an IG for CDA. This may include the care plan. The CDA R2 has a care plan model. May need to add entry level templates to meet needs.
- Should the end-point be a CDA schema gives the construct for a report. This is in addition to an IG.
- Decision: Perform a gap analysis of the CDA developing a C-CDA Implementation Guide and schema for the form.
- Child Health will adjust the PSS and return for a vote.
Patient Care WGM, Wednesday, May 7, 2014
- Back to Patient Care
- Back to 2014 PCWG WGM Agenda and Minutes
Patient Care Wednesday Q1
Patient Care hosting:
Present:
Elaine Ayers (Chair)
Iona Thraen (Scribe)
John Roberts
Russ Leftwich
Mitre Roche ONC
Agelie Cortez
Kevin Coonnan
Ed Hammond
Michael Tan
Anita Walden
Amil Popat
Patti Aymond
Jim Mcclay
Laura Heerman
Angelique Cortez
Evelyn Gallego
Marie Swall
Minutes:
- CIC
- - Publish Skizophrenia and major Depressive DAM
- - Working on Tuberculosis DAM
- - Issue of whether DAM is the best tool for modeling, New ways of capturing clinician input should be considered
- - Partnering with Tool committee to extract information from Enterprise system and EHR
- - CDA EMS went normative
- - CDA Trauma is DSTU
- BRIDG new working group, CIC will work with BRIDG to determine relationship and collaborations
- - FDA, NCI, HL7, CDISC BRIDG.org
- - BRIDG is brought back to HL7
- - Introduced to ISO
- - Question of intellectual property
- - Working with CBCC to harmonize Behavioral Health – Lori Simon
- - Differences and redundancies are contained across DAM
- - CIC was formed to bring clinical folks in to protect against technical algorithms
- - Need to bring Patient Care and CIC together, Boundaries are fuzzy
- - Need to understand band width of both group
- - Waiting to see where the FHIR opportunities are
- PHER
- - Echo fuzzy boundaries with CIC, Patient Care
- - Spend time reacting
- - Thank you for the TB DAM
- - 4 projects
- - Public Health Function
- - Working on joint effort with emergency management – bridge from Ambulance of OASIS and HL7 world
- - Includes hospital evacuation
- - Up to ears in help desk – authored and reviewed FAQ, knowledge based articles,
- - TSE – defining a workable relationship between where help desk staff can go for secondary backup when answers are not found, go to workgroup co-chairs
- - Confusion on what goes on lists serves than what should go to help desk to increase resources
- - Overlap between OASIS and other standards
- - Confusion on what goes on lists serves than what should go to help desk to increase resources
- - Immunization Resource and FHIR
- - Should this meeting be held next meeting?
- - Lots of development outside of HL7
- Emergency Care
DOM out for ballot – 70 comments DEED and DAM – issues related to the relationship Construction functional profile – took to CCHIT How is functional model vs functional profile used? Do they blend in to the certification? How related to conformance testing? Not on radar. Thrust of conformance testing is focused on Interoperability. Does ONC have certification? Yes Office of Science and technology have certification groups. With HITECH standards have put criteria by HL7 has been put aside. EHR functional model Implementation are an intervention and small group trying to determine use ability criteria. Important to the end user. How to create framework around useability, trying to determine conformance criteria, Meaningful use conformance criteria has been balloted
Vendors need functional profile.
Evaluating and writing to raise awareness
- Patient Care
- - Care Plan DAM has been balloted in second cycle and is being reconciled
- - Care Coordination Services Functional model in second cycle and is being reconciled
- - Health Concern previous DSTU was withdrawn, coordinating with overlapping material
- - New Health Concern DAM project in progress
- - Allergy intolerance DAM successfully balloted, working on terminologies for non medication substances,
- - Working with ISDO to close gaps
- - Working on harmonization list in CDA
- - Two efforts
- - Providing clinical input to FHIR
- - Co sponsor portable health record for children with special health care needs
- - Asked to develop FHIR resources on referral
- - Added 7 new projects associated with FHIR
- - Question
- - How much of this is a duplication with EHR? Recommend consolidation with EHR.
- S & I Report
- - Asking for regular update to HL7 will bring feedback to
- - SDC is going to ballot and effects implementation
- - Recommend that the report be standardized.
- - Asking for strategy for report out
Patient Care Wednesday Q2
PCWG representatives to present updates to EHRWG
Present:
Stephen Chu
Laura Heermann Langford
Elaine Ayres
Iona Thraen
Jay Lyle
Enrique Meneses
Kevin Coonan
Minutes:
Contents/details of PCWG updates - see the following slide deck:
Patient Care Wednesday Q3
Patient Care hosting: SOA and Patient Administration (PA)
Present:
Stephen Chu (chair)
Iona Thraen (scribe)
Enrique Meneses
Michael Tan
Jay Lyle
Kevin Coonan
Ken Rubin
Iryna Roy, Yonggian Bao
Michelle Osborne
Alexander DeLeon
Irma Jongeneel
Brisn Postlethwaite
Russell Leftwich
Minutes:
- SOA and Patient Administration updates on:
- - interconnectivity registry project and human services directory project follow up from San Antonio
- - Several years ago, service and provider directories, human services directories communication.
- - This is the same the human services directory project proposed by Australia
- - Healthcare and human services provider directory went through as normative
- - Need to review the specification based on implementation experience
- - Question of NIEM connectivity to human service directory
- - Discussions:
- - This project was previous processes through CBCC
- - CBCC was previously under patient care which is why this project is considered to fall under patient care
- - Question: whether Patient Care has interest to be home for human services directory project
- - PC expresses the human services directory project may have use for referral project but has no resources to take ownership
- - PA is recommended to be home for this project and agrees to take over this project
- - Discussions:
- - Interconnectivity registry project
- - DAM was produced for this project and balloted
- - contains architecture and functional contents
- – was not reconciliation (3-4 Yrs) ago: March 3, 2011
- - Many calls for participation has not gotten much response for the interdependent registry
- - Patient care has no real interest or expertise
- - Pt admin is recommended as project home
- - PA recommends this project be closed as there is no further work done on this project
- - DAM was produced for this project and balloted
- - Discussions:
- - It was suggested that this project might be useful for/relevant to care coordination; but PC has no bandwidth
- - Enrique offered to review documentation and to determine components that may be relevant to care coordination
- - then to recommend what to do
- - Discussions:
- - Decision
- - PA will own interdependent registry work
- - Enrique will review interdependent registry document to determine areas of relevance and to make recommendation
- - PA will own human services directory work
- - Putting together FIHR resources for healthcare service directory and harmonizing
- - PA will own interdependent registry work
- - Decision
- Future WGM joint meeting discussions:
- - Question on whether there is future need for PC to host SOA in WGM
- - Given that CCS project is likely to conclude by September, there may not be a need for PC to host SOA
- - SOA reps can be invited to join PC meeting on a need basis
- - SOA will check and confirm
- - Question on whether there is future need for PC to host PA in WGM
- - PA is Working on Episode of care which may need PC inputs
- – But there is unlikely to need to schedule joint meeting
- - PA will post to the patient care group mailing list to keep PC informed. Usually do the work on conference calls.
- - Have PA FHIR site
- CCS ballot reconciliation:
- - Negatives – Reconciliation
- - p. 28 Persuasive with Mod, Change statement to acknowledge receipt by recipient
- - Patient consent: Is acceptance review different from patient consent? Consent creates a legal burden, change to patient acceptance. Non persuasive in that it is covers by patient acceptance and not consent. Consider changing review acceptance into care team acceptance. Functional capability is covered by acceptance review and changed to team acceptance. This raises questions about where the acceptance process would be done by service. Setting parameter or flagging.
- - p.38 non persuasive
- - Block vote: 7 (affirmative); 0 (abstain); 0 (against)
- - Remaining ballots comments to be resolved during conference calls
Patient Care Wednesday Q4
Present:
• Elaine Ayres (Chair)
• Michael Tan ( Scribe)
• Stephen Chu
• Christina Knotts
• Kevin Coonan
• Lisa Nelson
• Lindsey Hoggle
• Cathy Welsh
• Brian Scheller
• Martin Rosner
• Jay Lyle
• Margeret Ditloff
• Rob Hausam
• George Cole
• Enrique Meneses
• Vassil Peytchev
• Brett Marquard
Minutes:
Allergy/Intolerance and Adverse Reaction updates and discussios
• The Allergy/Intolerance and Adverse Reaction DAM is published.
• The Clinical Model has been balloted in September 2013. It has to be republished.
• Further work:
- o We need to develop terminology and value sets
- o Also test models.
• On terminology:
- o Food and Nutrition are based on the VA list. Need to submit additional terms to US extenstion. See slide SNOMED-CT versus UNII.
- o There is a 1.1 version and r2
- o Glossary SKMT needs to add harmonization. This is orginally from Canada Health Infoway.
- o Question about the hierarchie of value sets whether this is a recommendation or a priority. Brett thinks it is more a recommendation. You can send other values.
- o The food allergies is from unii, but there are issues. ( for example shell fish).
- o A Terminology PSS was taken by Rob to Vocab and there were a lot of comments.
- - These questions are still outstanding. The PSS is not yet approved.
- - The work will still be done, even without a PSS, but the risk is that the drive will be gone.
- - There is a project dependency on ITHSDO to provide new SNOMED -CT codes.
- o According to Russ we do need to clean up the allergy tree.
- o Russ moves to continue with the project as stated in the PSS project 1086 . Second by Rob Hausam.
- o Vote: 15 in favor, 2 abstain, 0 against.
• FHIR model:
o There is a code set for criticality: The FHIR resource contains: fatal high medium w..
o In the Netherlands there are 4 values.
o In Australia they have decided not to use severity and only use absolute criticality.
o Stephen suggests to remove the current code and use a SNOMED code:
3 code system: critical and not critical and unknown.
Does it use the negation indicator? In FHIR there is no negation indicator.
o Russ places a motion to change the list to a 2 code system.
o Rob suggests to amend the motion to decide only to say that the current list is not be used and we should evaluate for a proper value set.
o Vote: 17 in favor, 1 abstain and 0 against.
• Allergy/Intolerance, Adverse Reaction Model - C-CDA templates alignment analysis:
- o Lisa Nelson has compared CCDA the allergie templates in Consolidated CDA 1.1. There are 2 templates but only 1 with entry. There is an Allergy Intolerance Observation.
- o Most of the discussion is about the appearance of severity in 2 places. One is actually the criticality. The suspicion is that most system use the severity of the reaction as a criticality.
- o CCDA has identified SNOMED-CT codes to use in CCDA.
- o Is an adverse event used in CCDA the same as adverse reaction ?
- o Lisa has compared the model of PCWG with the model from CCDA and made visible what the differences are.
- o According to Lisa there is an inversion between the reaction and the concern, but this could not be found anymore.
- o On the other hand CCDA has other templates for other procedures that are not available in the PCWG model.
- o There is a difference between the status of an observation and the clinical observation.
- o Lisa will put the differences in a list and add them as comments to a ballot and resolve them together with Structured Docs.
- Allergy/Intolerance, Adverse Reaction Alignment analysis slide deck from Lisa Nelson is available here:
Patient Care WGM, Thursday, May 8, 2014
- Back to Patient Care
- Back to 2014 PCWG WGM Agenda and Minutes
Patient Care Thursday Q1
Present:
• Elaine Ayres (Chair)
• Michael Tan (Scribe)
• Russel Leftwich
• Jay Lyle
• Iona Thraen
• Patrick Loyd
• Mead Walker
• Mark Shafarman
• Enrique Meneses
• David Burgess
• David Hamill
• William Goosen
• Larry McNight
• Laura Heermann
• Jim McClay
• Ken McCaslin
• Brian Scheller
• Clem McDonald
• Ed Hammond
• Stephen Chu
• Kevin Coonan
• Anita Walker
• Atanu Sen
• Mark Roche
• Vijay Shah
• Bron Kisler
• Mitra Rocca
• Rebecca Kush
• Shreya Soni
• Leslie Tompkins
Minutes:
- Electronic Services: common data element repositories
- - There seem to be many common data element repositories; we endeavor to identify some of them and characterize the “CDE”s they contain.
- 1. ONC: S&I Framework has a project called Structured Data Capture that is sponsoring a project to create a FHIR resource called Observation Definition. This project will also create a set of profiles which are essentially CDEs.
- 2. NIH has a portal at nlm.nih.gov/CDE. It includes definitions and classifications (e.g., universal vs. domain-specific; required; core).
- a. This repository uses some of ISO 11179, but not where 11179 properties are specific to a technical implementation.
- b. NLM specifies information necessary to define a data element; it includes provenance, codes, units.
- 3. NLM has the Value Set Authority Center (VSAC). This is for value sets, not data elements.
- a. We need a standard way to define value sets.
- 4. National Cancer Institute’s CADSR follows 11179.
- a. CIC uses these in DAMs because of its accessibility.
- 5. LOINC
- 6. CDISC
- a. A research data set of fewer than 200 elements, agreed by all ICH countries.
- Data element definition
- - There are very many organizations that are creating or aggregating elements or value sets. The problem is not a lack of common data elements, but the fact that they are not commonly reused.
- - There is a question of how much context a CDE needs to specify. The less context is included, the more general and reusable the CDE is. Many definitions contain extraneous information that impedes reuse. Some cases do require more specific concepts: “race” values for demographic purposes differ from those used for clinical purposes. But the value of a CDE is the “common” part to support reuse: these desiderata are in conflict, and it would be beneficial to develop common principles for resolving that conflict.
- - There is a need to encourage or enforce reuse; NLM may include such a requirement in future grants.
- - Governance
- o NLM does not at this time have authority to modify contributions to CDE, even if they are of low quality. This threatens to make the repository too large and messy to be useful.
- - What is the right place to store CDEs? We need to define our needs in order to identify the right place. It may be possible to adopt a federated model, where the many repositories are coordinated.
- The ONC’s S&I framework Structure Data Capture porject
- - The project team has proposed a project scope statement to
- 1. define a syntax for CDE definition (conforming to 11179)
- a. Using a controlled terminology to specify semantics
- 2. create a FHIR resource to represent the CDE (Observation Definition)
- 3. create FHIR profiles of that resource to express the semantics of the CDEs
- 1. define a syntax for CDE definition (conforming to 11179)
- - The minimum set of CDEs is defined by Meaningful Use 2, which is the driver for the project. These will be hosted and curated by HL7. Other organizations may define their own; NLM will create an interface to consolidate references to a federated set of repositories.
- - A question was raised as to why the proposed modeling approach does not leverage the DCM specification. The ensuing discussion centered around the respective approaches to model composition and failed to answer the question.
- - A question was raised as to a strategy for normalizing naming conventions.
A question was raised as to why CADSR was not used. The response suggested that the team believed that CADSR is for research and may not be used : - for clinical elements. Several attendees disagreed.
- - A question was raised as to where Meaningful Use specifies terminology bindings. The S&I team responded that they will provide this information.
- - A question was raised concerning HL7’s role.
- - Repositories may have specific purposes, so there may be many, but HL7 should encourage consistent metadata.
Like CDA, it seems that a tool designed to be an implementation specification is inadvertently specifying clinical content. It is not clear that there is a source of clinical definition for these profiles independent of the profiles themselves. The workgroups agreed to reserve this meeting slot for September
- PCWG reporting to OO and CDS
- - Stephen Chu attended the joint OO, PCWG and CDS meeting (OO hosting)
- - CDS did not attend
- - Stephen provided report/updates on PCWG projects:
- o Allergy/Intolerance and adverse reaction
- o Care Plan
- o Card Coordination Services Functional Model
- o Referral and Transition of Care FHIR resources
- o FHIR clinical resources maintenance
- o FHIR clinical connectathon
- o PCWG co-sponsored projects include SDC project
- - Stephen returned to PCWG meeting after completion of updates
Patient Care Thursday Q2 (PCWG, SDWG, Template Joint meeting)
PCWG hosting Structured Doc and Template
Present:
Stephen Chu – chair
Elaine Ayres – scribe
Lisa Nelson
Jay Lyle
Iona Thraen
Mark Shaferman
Kai Heitmann
Enrique Menses
Sarah Gaunt
Rick Geimer
Mead Walker
Austin Kreisler
Lindsey Hoggle
Tim McNeil
William Goossen
David Hay
George Cole
Matt Rahn
Shreya Soni
Larry McKnight
Vanayak Kulkaray
Michael Tan
Marie Swall
Martin Rosner
Brian Scheller
Brett Marquard
Sean McIlvenna
Minutes:
- Templates:
- - Templates asked to have additional information on “CDA on FHIR”.
- o This is a universal profile for CDA – clinical documents. There may be extensions. There is a C-CDA to FHIR mapping work as a parallel work product. Is there a need for Templates to review?
- - Patient Care has a PSS for a Referral Resource.
- - Templates WG is leading a project with CGIT (Conformance and Guidance) to ensure that FHIR profiles can support what Templates need for expression.
- o Is there a joint PSS that should be created for expression of templates in FHIR with SDWG, Templates and Patient Care?
- o Trifolia is working on expressing CDA in FHIR in a FHIR profile syntax.
- - The output would the definition of a CDA template and make sure that the FHIR profile has all of the templates functionality.
- - Templates (DSTU) already aligns to C-CDA meta data, but not fully aligned with FHIR.
- o Patient Care would agree to be an interested party with the meta-data aspect of this relationship.
- Patient Care:
- - PSS for Referral and Transitions of Care FHIR Resource is a new project for Patient Care.
- o Will have clinical and administrative data elements for referral and response.
- - Allergy and Intolerance project – update DAM now published, Clinical Models will be published shortly.
- o PC now harmonizing with C-CDA R1.1 to ensure that concepts are equivalent, specifically the concept of criticality (which is expressed as severity in C-CDA).
- o Will also require updates to the Value Set definitions and additional concepts to express environmental and food substances in SNOMED-CT. The issue of “status entry relationship”.
- o In R2 there is no status entry relationship, and PC does use this.
- - There is the status of the clinical condition itself vs. the status of the observation.
- - SDWG C-CDA draft for comment will be published this evening but PC should take a look at this document for comment.
- - Care Plan in C-CDA R2 – templates were developed with the Care Plan DAM. However there have been changes in the Care Plan.
- o This will require further harmonization between SDWG and PCWG.
- o Ballot comments on both projects will need to be addressed.
- o The Care Plan DAM is anticipated to be published in the September WG time frame.
- - Health Concern – the concept is in C-CDA but PC is revisiting the topic to better define.
- o PC WG will ballot a DAM for the September 2014 ballot.
- o What is the relationship of the health concern vs. the concern thread (tracking)?
- o How are these concepts related to the health concern event?
- SDWG:
- - Issue related to Performer participation – roles on the health care team?
- o Performer type and role code – filled by the NUCC role taxonomy.
- o Performer, participation and function needs additional guidance re care team members.
- - How do you differentiate between role and participant codes?
- o Are we trying to represent care team provider where it is not necessary?
- o There is a new use case – can create a new participant (generic).
- o The patient care DMIM allows for a generic participant, including a patient as an author.
- o The function code is “CWE” and additional values may need to be added. However, the service event act drives the correct use of the participant.
- o In the errata publication there appears to be an error in participant mnemonic (PP instead of PCP).
- o Is there an intended difference between PP (Primary Physician) vs. PCP (Primary Care Physician?
- Future WGM joint meeting:
- - PCWG, Structured Doc and Template agreed to continue joint meeting: Thursday Q2
- - PCWG will host
Patient Care Thursday Q3
PCWG attending CS meeting
Present:
Stephen Chu (scribe for PCWG)
Russ Leftwich
Michael Tan
William Goossen
Minutes:
- CS CMET – ballot reconciliation
- - Affirmative vote with one comments on typo to be fixed by editors
- - Motion to accept ballot disposition and to publish CS CMET (motion passed)
- - CS R2 and CMET are now normative
- - Both transit into maintenance
- International template for patient summary in CDA – patient summary form will accompany patient when travelling and use when necessary
- - Output of this project: document templates based on CDA R2
- - To include minimal required data
- o Looked at patient summary from US
- o And patient summary from epSOS
- o Picked the overlaps (sections)
- - Areas outside the overlap will be discussed during international conference calls
- - Question raised on methodology which may possibly lead to omission of important clinical data components/sections
- - Any issues/concerns to be dealt with by post WGM conference calls
- - PCWG will be interested party
- - wiki and email information to be sent to PCWG co-chairs
- Future WGM arrangement with PCWG
- - PCWG will send delegate to CS meeting if there are agenda items that concern PCWG
- - PCWG will retain this quarter for PCWG specific agenda items (i.e. CS does not need to host PCWG)
Patient Care Thursday Q4
PCWG meeting: review and approve CHWG PSS; Health Concern topic discussions
Present:
Stephen Chu (Chair)
Kevin Coonan
Michael Tan
Larry McKnight
Galen Mulrooney
Russ Leftwich
Jay Lyle
Elaine Ayres
Minutes:
- Trillium Bridge PSS – International portable health record. Patient Care will be an interested party. SDWG is the sponsor.
- PSS for Essential Information for Children with Special Health Care Needs. Child Health WG is the sponsor.
- • PC recommends that the PSS includes an Emergency Care SME.
- • Also recommend that in Project Scope be amended – a schema be changed to required templates, and electronic format (e.g. CDA)
- • Advanced directive should be “Advance directive”.
- • In 3C Success Criteria - Development of a standardized electronic format…
- • In 3D – change form to format
- • Complete DSTU - update date
- • NIB – Nov 6, Final Ballot Materials Submission – December 1, 2014
- • Complete Ballot reconciliation March 2015
- • Publish DSTU May 2015
- • Submit first normative ballot November 2017
- • Complete normative ballot reconciliation March 2017
- • Publish normative R1 May 2017
- • Project end date May 2017
- • Check Implementation guide, uncheck amend existing standard.
- VOTE: Motion to approve with editorial comments: Galen/Russ
- Oppose – 0, Abstain – 1, In favor – 6
- Health Concern Topic
- - The mind map requires review by clinicians.
- - Most EHR’s are creating a problem, there is no abstraction layer that tracks this over time. When sent there is no qualification.
- - Note that C-CDA has a health concern and a problem concern. These terms were trying to represent a condition such as a pregnancy where it is not a problem…..
- - A problem with a number is essential a tracked problem. When sharing, can “subscribe” to that concern if you wish to track and follow.
- - In CDA – the “health concern” is represented as an observation with a status of “complete” with a wrapper of concern ID to track (this is an extra XML tag). Not clear how CDA does grouping. A grouping can be a list of problems, e.g. Diabetes. The concern acts as a grouper for the Diabetes thread. When passing in CDA – only pass one observation e.g. Diabetes, a list of one element.
- - Suggest adding a use case related to pregnancy.
- - The mind map conceptual model is now stable.
- - Are previous models useable (DMIM/RMIM)? How is the concern updated over time?
We need to be clear between the Act Event and Observation Event. Is the Observation Event the Health Concern and the Act Event the tracker?
- - All of these issues were discussed in the 2008 ballot….Concern is the Act, and the naming came in a “Care Statement”. The sets are groups of care statements. The model also relates concerns and nests concerns… However, the model is generic and needs to be constrained.
- - Would suggest adding attribute of “name” as an observation to modify concern.
- o Larry has a concern tracking slide deck.
- o “Concern” wraps an observation.
- o The name of the concern is taken from the last observation – because the condition would evolve over time.
- - Discussion on: Existing Concern R-MIM needs to be revised to include this capability to express the Concern name at a specific point in time
- o Question – add “name” to concern act box. Need rules to define how to manage the “name” over time. The concern is renamed, not changed.
- o Are these names symptoms or diagnoses? These are blurry, and there may not be a diagnosis..
- - Next steps – Conference calls.
- 1. There are adequate use cases at this point but need to revisit
- 2. Do we need a logical model or can we use the conceptual model?
- 3. Revisit the RMIM from 2008.
- 4. Conference calls on Thursday 4 PM EDT every two weeks. Michael will set up calls.
Patient Care WGM, Friday, May 9, 2014
- Back to Patient Care
- Back to 2014 PCWG WGM Agenda and Minutes
Patient Care Friday Q0: PCWG Co-Chairs meeting
Present:
Elaine Ayres (Scribe)
Stephen Chu
Michael Tan
Laura Heermann Langford
Russ Leftwich
Minutes:
Patient Care Friday Q1
Present:
Minutes:
Patient Care Friday Q2
Present:
Minutes:
Patient Care Friday Q3
- PCWG - no meeting this quarter
Present:
Minutes:
Patient Care Friday Q4
- PCWG - no meeting this quarter
Present:
Minutes: