Difference between revisions of "Coordination of Care Models"
| Line 1: | Line 1: | ||
| − | [[category:Patient Care]] [[category:Coordination | + | [[category:Patient Care]] [[category:Care Coordination Service]] |
[[File:go_back.png|32px|link=Care Coordination Service]] | [[File:go_back.png|32px|link=Care Coordination Service]] | ||
| − | '''Return to:''' [[Care | + | '''Return to:''' [[Coordination of Care Services Specification Project]] '''or''' [[ Care Plan Project]] |
<p> | <p> | ||
The composition of the care team is determined by jurisdictional, organizational, credentialing body policies, and financing mechanisms. Further, it may vary based on the patient’s personal and/or family’s choice (often within the constraints of the various policies and financing mechanisms). This section assumes the existence of a care team with the goal of establishing the context of ongoing and incremental contributions to the care plan and associated care data. The patient and family are assumed to be part of the care team. A key assumption is that all members of the care team are aware of each other, have been authorized to access the care plan. It is also assumed that each member of the care team is accessing the care plan and coordinating care through a system which implements a specification derived from the service functional model described in this document. | The composition of the care team is determined by jurisdictional, organizational, credentialing body policies, and financing mechanisms. Further, it may vary based on the patient’s personal and/or family’s choice (often within the constraints of the various policies and financing mechanisms). This section assumes the existence of a care team with the goal of establishing the context of ongoing and incremental contributions to the care plan and associated care data. The patient and family are assumed to be part of the care team. A key assumption is that all members of the care team are aware of each other, have been authorized to access the care plan. It is also assumed that each member of the care team is accessing the care plan and coordinating care through a system which implements a specification derived from the service functional model described in this document. | ||
Latest revision as of 17:01, 6 May 2014
![]() Return to: Coordination of Care Services Specification Project or Care Plan Project
Return to: Coordination of Care Services Specification Project or Care Plan Project
The composition of the care team is determined by jurisdictional, organizational, credentialing body policies, and financing mechanisms. Further, it may vary based on the patient’s personal and/or family’s choice (often within the constraints of the various policies and financing mechanisms). This section assumes the existence of a care team with the goal of establishing the context of ongoing and incremental contributions to the care plan and associated care data. The patient and family are assumed to be part of the care team. A key assumption is that all members of the care team are aware of each other, have been authorized to access the care plan. It is also assumed that each member of the care team is accessing the care plan and coordinating care through a system which implements a specification derived from the service functional model described in this document.
This section describes the context and pattern of collaboration and interaction paths rather than a fixed process. Coordination of care is framed from the perspective of dynamic evolution of care driven by ongoing evaluation of the patient’s health status and collaboration of the dare team. The care team is assumed to have a shared awareness of the changing care plan which is automatically synchronized to all members as it is changed, so as to surface awareness for the need to reconcile and adjust care when new or conflicting information becomes available. Synchronization of the care plan eliminates gaps in information and breakdowns due to missing change updates, conflicting information, and incorporation of new findings. Synchronization can also exposes inconsistencies and helps resolve conflict between specialty views of the plan; helping determine the need for expert clinical reconciliation. It shares information across what previously has been isolated corners of the care continuum.
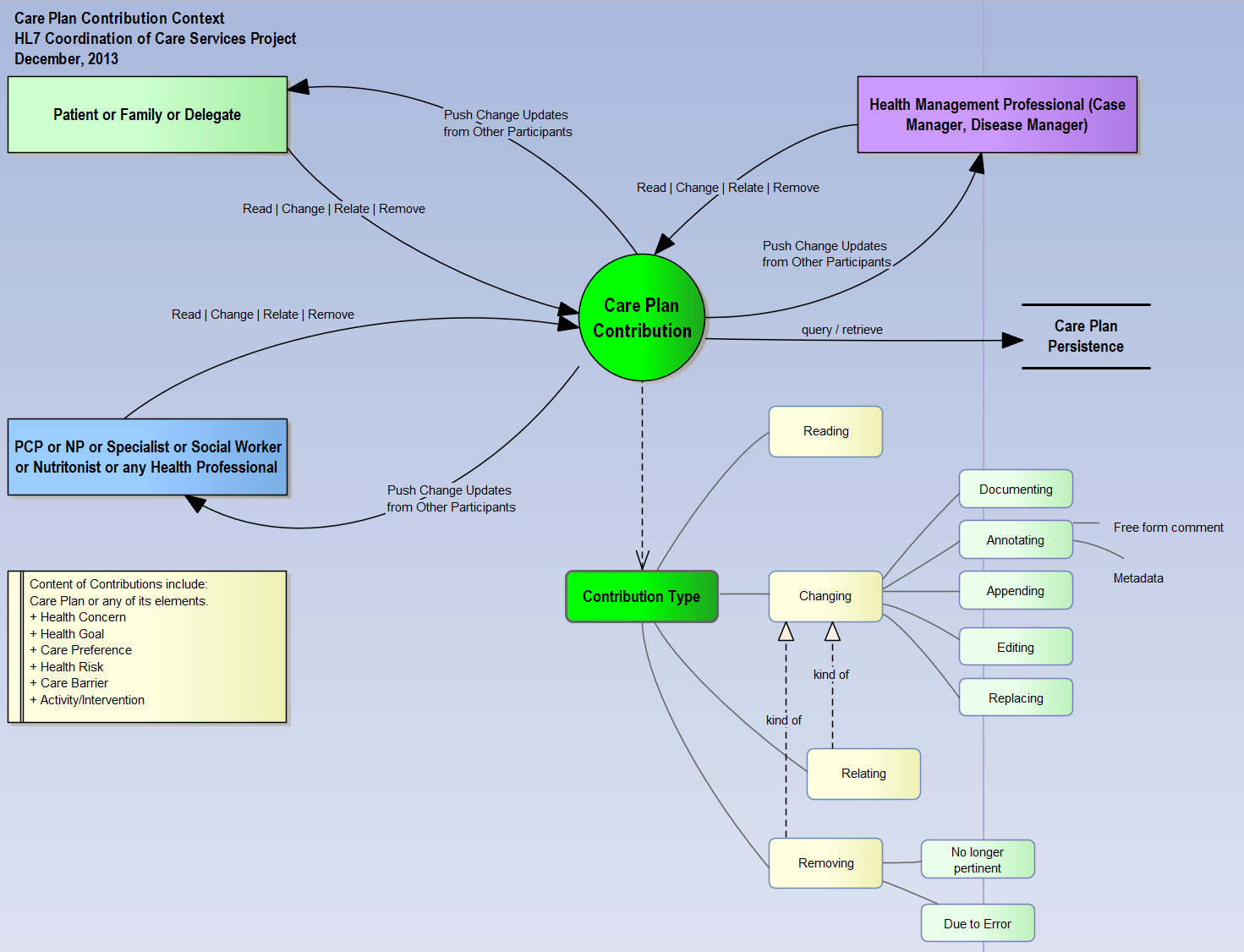
The context of care team contribution starts with: Any care team member can “say” anything pertinent at any time resulting in change updates to the shared/synchronized content and resulting in notification to other care team members who in turn can react to the changes. Contribution may result in changing structured elements of the plan, health concerns, health goals, care preferences, health risks, health barriers, or the status and documentation of care activities and interventions. Care team contribution is controlled by the dynamic ongoing negotiation of care team members who may accept, reject and propose alternatives. There are other controls to care team contributions based on organization business rules and policies which are out of the scope of this specification. This specification focuses on the roles of the team members, autonomous decision making, and interaction of individuals who are acting on shared and synchronized content.
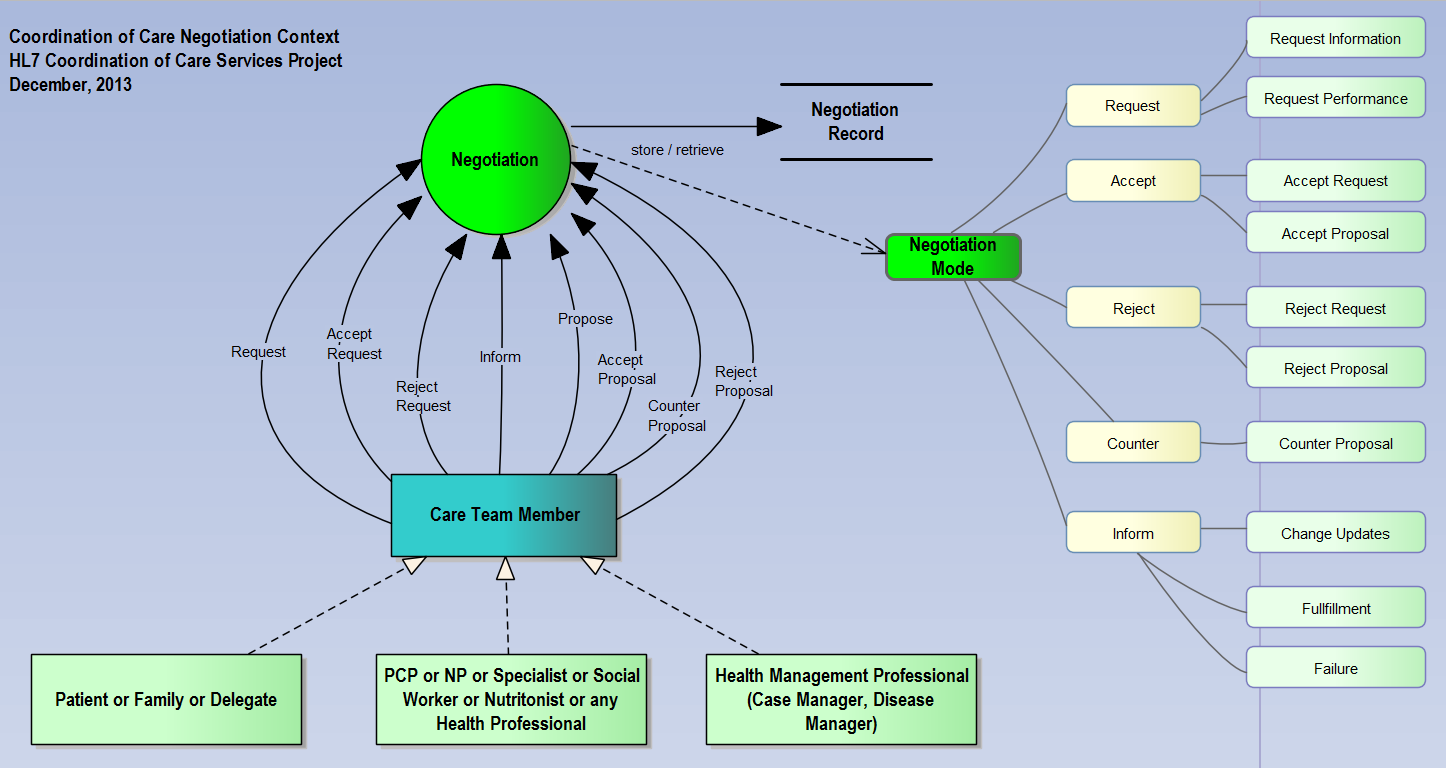
Central to collaboration is the concept of negotiation. Care Team negotiation consist of an emergent and dynamic flow of interactions between two or more individuals as they inform each other, make requests, and make proposals. It also includes actions to accept, reject or counter the requests and proposals in order to reach agreement. It is expected that clinical decision support system agents will also participate in negotiation by proposing, informing and counter-proposing.
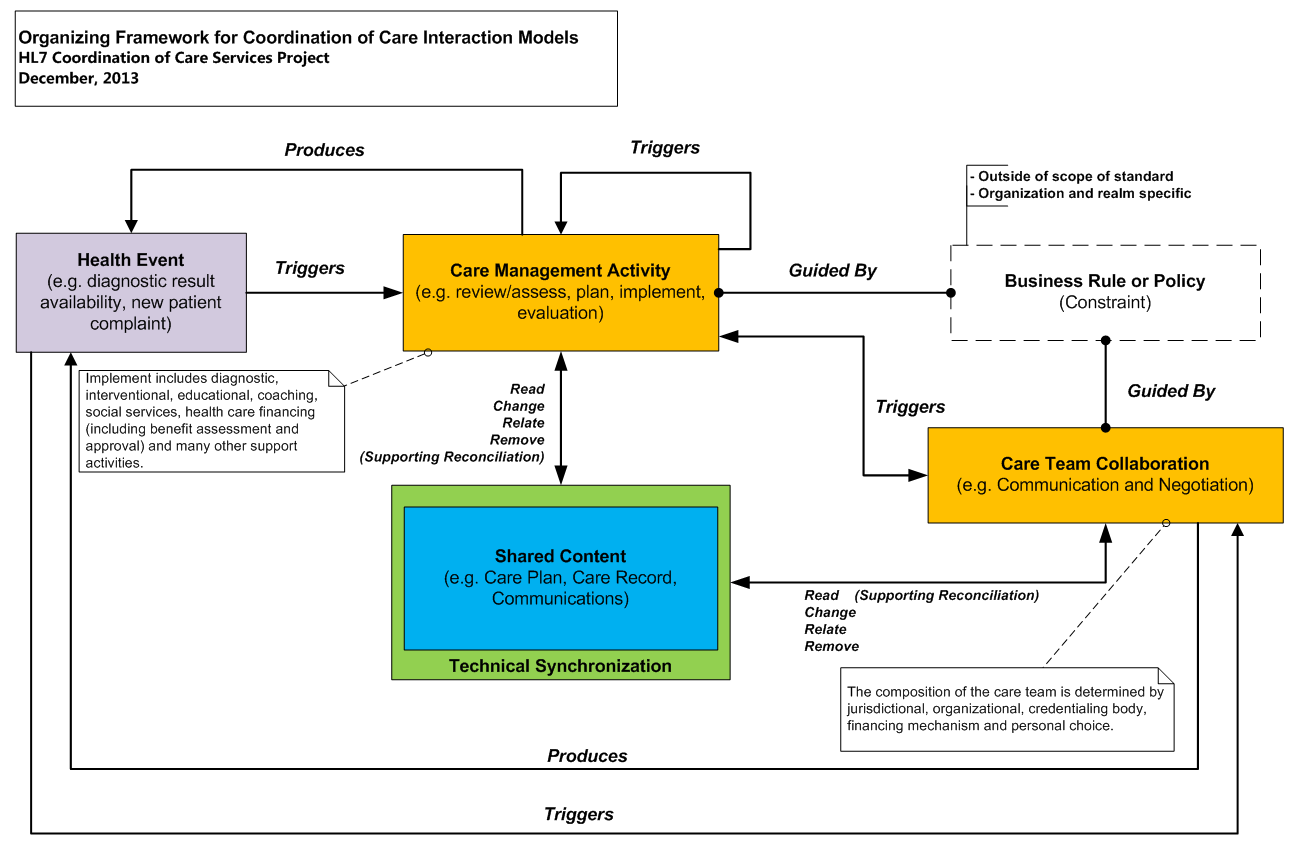
The diagram in figure 5 provides an organizing framework for coordination of care dynamic models. It may be viewed as a meta-model for coordination of care interaction and collaboration models. The organizing model establishes the relationships between Health Event, Care Management Activity, Care Collaboration and Shared Content. Shared Content consists of the care plan and other associated information content. Shared content is synchronized among care team participants. The main idea is to support shared care team awareness and transparency of the patient’s care in order to eliminate gaps, redundancies and conflicts in the information and in the care process. Shared content is updated at various stages of interaction (including synchronization, harmonization, post negotiation) leading to self-organizing and reconciled systems. Shared content is incrementally created as a result of ongoing interactions.
A Health Event is an occurrence of importance to the health of the patient. The event may result from a change in the patient’s physical, socio-economic status reported by the patient/family, or change in information or knowledge resulted from care management activities or from care team collaboration and interactions, which is often or should be directly recorded. The event in turn may trigger new care management activities or new collaborations and interactions which in turn result in incremental updates to the shared content and context.
A Care Management Activity is the act of developing care strategies and the performance of tasks (which includes investigations, interventions and evaluations) in support of patient’s care by one or more care team members. Care management activities are indicated in the plan.
Care Team Collaboration emerges during the evolution of care team evaluation, decision making and autonomous direction within the constraints of professional standards, policies, business rules, care team working agreements and social contracts.
Business rules and policies are out of the scope of this specification. The meta-model simply acknowledges their existence and their relationship as a constraint in guiding care management activities and care team collaboration. Coordination of care systems would make available their model content and context to support decision making based on business rules and organization policies. The model content corresponds to the input and outputs defined in the capabilities defined in this document and the model detailed in the HL7 Care Plan DAM.
A view of the dynamic, ongoing and emergent care team contribution based on a shared care plan may look as follows:
- A care team member looks up an existing plan
- A plan may be created if none exists or its existence is not known
- The plan changes based on the care team member’s assessment with the patient
- Health goals, care preferences, health concerns, health risks, care barriers, care activities and interventions are assessed, validated, added, changed or removed.
- The plan leads to a cycle of intervention, outcomes and review
- The patient may be referred to a specialist or other health and social services providers
- The care team member requests participation from the specialist or other providers and subsequently shares the plan
- As the patient transitions to the specialist or other health provider care settings the care event steps can be repeated with the actors represented by the generic “care team member”
- Communication may occur at any time between care team members as they react to synchronized content change updates.