Assessment Scales
There is work underway for a new R-MIM on scores and assessment scales. This page provides the material which will be used for the next ballot cycle. Patient Care has agreed to bring it to ballot as DSTU. So please feel free to support this initiative by providing additional input.
This paper will be organized according to the following three components:
- Rationale for paying attention to assessment scales / scores / indexes as a separate topic
- The HL7 v3 ballot material persé: use cases, storyboards, dynamic model, static R-MIM model.
- Instructions for use to define assessment scale as Detailed Clinical Model, including the coding of it, and use it against the care statement / assessment scale R-MIM.
Contents
- 1 Contributors
- 2 Introduction
- 3 1. Intensive Care and Anasthesia
- 4 2. Patient Care
- 5 3. Psychiatry and Psychology
- 6 4. Pediatry
- 7 5. Mobility
- 8 6. Cognition
- 9 7. Nutrition
- 10 8. Psychology
- 11 9. Geriatry
- 12 10. not otherwise classified
- 13 Foundation
- 14 Storyboard
- 15 Application Roles
- 16 Trigger Events
- 17 Refined Message Information Models
- 18 Walkthrough
- 18.1 Class Score
- 18.1.1 classCode := OBS
- 18.1.2 moodCode <= ActMoodCompletionTrack
- 18.1.3 id (Score-ID) := SET<II> [1..*]
- 18.1.4 code (score system) := CD CWE [1..1]
- 18.1.5 derivationExpr (calculation method) := ST [0..1]
- 18.1.6 statusCode (Status) := CS CNE [1..1] <= ActStatus
- 18.1.7 effectiveTime (observation time) := GTS [0..1]
- 18.1.8 availabilityTime := TS [0..1]
- 18.1.9 priorityCode := SET<CE> CWE [0..*] <= ActPriority
- 18.1.10 confidentialityCode := SET<CE> CWE [0..*] <= Confidentiality
- 18.1.11 uncertaintyCode := CE CNE [0..1] <= ActUncertainty
- 18.1.12 languageCode (language) := CE CWE [0..1] <= HumanLanguage
- 18.1.13 value (total Score Value) := ANY [0..1]
- 18.1.14 interpretationCode (Interpretation) := SET<CE> CWE [0..*] <= ObservationInterpretation
- 18.1.15 methodCode := SET<CE> CWE [0..*] <= ObservationMethod
- 18.1.16 targetSiteCode := SET<CD> CWE [0..*] <= ActSite
- 18.2 Class ScoreItem
- 18.2.1 classCode := OBS
- 18.2.2 moodCode <= ActMoodCompletionTrack
- 18.2.3 id (Score-ID) := SET<II> [0..*]
- 18.2.4 code (score system) := CD CWE [1..1] <= ActCode
- 18.2.5 negationInd := BL [0..1]
- 18.2.6 text := ED [0..1]
- 18.2.7 statusCode (status) := CS CNE [1..1] <= ActStatus
- 18.2.8 effectiveTime (observation time) := GTS [0..1]
- 18.2.9 availabilityTime := TS [0..1]
- 18.2.10 priorityCode := SET<CE> CWE [0..*] <= ActPriority
- 18.2.11 confidentialityCode := SET<CE> CWE [0..*] <= Confidentiality
- 18.2.12 uncertaintyCode := CE CNE [0..1] <= ActUncertainty
- 18.2.13 languageCode (language) := CE CWE [0..1] <= HumanLanguage
- 18.2.14 value (score value) := ANY [0..1]
- 18.2.15 interpretationCode (interpretation of the value) := SET<CE> CWE [0..*] <= ObservationInterpretation
- 18.2.16 methodCode := SET<CE> CWE [0..*] <= ObservationMethod
- 18.2.17 targetSiteCode := SET<CD> CWE [0..*] <= ActSite
- 18.3 Act-Relationship component
- 18.4 Participation performer
- 18.5 Participation author
- 18.5.1 author (Angaben zum Author) := [0..*]
- 18.5.2 typeCode <= AUT
- 18.5.3 functionCode (function of the author) := CE CWE [1..1] <= ParticipationFunction
- 18.5.4 contextControlCode := CS CNE [0..1] <= ContextControl
- 18.5.5 noteText := ED [0..1]
- 18.5.6 time (Zeitpunkt der Dokumentation) := TS [1..1]
- 18.5.7 modeCode := CE CWE [0..1]
- 18.5.8 signatureCode := CE CNE [0..1] <= ParticipationSignature
- 18.5.9 signatureText := ED [0..1]
- 18.6 Participation Unterzeichner
- 18.7 Participation verifier
- 18.8 Participation dataEnterer
- 18.9 Participation subject
- 18.10 CMET Choice Box
- 18.11 Act-Relationship referenceRange
- 18.12 class ScoreRange
- 18.1 Class Score
- 19 Hierarchical Message Descriptions
- 20 Dynamic Model
- 21 Open Issues
Contributors
Principal Contributor: Frank Oemig, Agfa HealthCare & HL7 Germany
Principal Contributor: William Goossen, MD
Principal Contributor: Kevin Coonan, MD
Principal Contributor: Sylvia Thun, MD, DIMDI
Principal Contributor: Rainer Röhrig, MD, University Hospital Giessen
Introduction
The most fundamental question is always how certain information in HL7 should be transmitted. In most cases, it is information that belongs to the category of "findings" or "observations". Therefore, in HL7 v2.x the OBX-Segment can be used. In HL7 V3 we will find some classes within the RIM and the appropriate domain models. Further it will deal with interpreting the score values and with implementing it in CDA documents and messages.
The so-called Score or assessment systems are findings. Score systems are so-called severity classification systems or point totals systems that pretend to make a quantitative statement on the severity and prognisis of a disease. Typically, scores combines individual values into a total which can be interpreted more easily. In the simplest case, it is just a single value or based on two individual values, in a complex case it can consist of several dozen values which are combined using a complex mathematical calculation.
This document tries to address two kinds of requirements. First, it should define which codes for the most important score and assessment systems must be used. On the other hand, it should explain how the information should be mapped to HL7 v2.x and V3.
Scope
There are many score systems in use ([Wikipedia]). Many systems are in use on an international, national or just hospitalwide level. Others are just for scientific purposes.
Codes
For our communication the following information are of interest:
- Code (how to identify the data?)
- Codesystem (what is the originating catalog?) – LOINC, alternatively Snomed CT, if a licences is available
- name + description (short textual description)
- value (information)
- unit
- interpretation
In addition to this information for an individual score the underlying values used for calculation are of importance as well. But these are based on the same 6 points mentioned above.
Application Domains
The score systems can be assigned to specific domains. The following table lists the score systems (in alphabetic order) per domain with the assigned code (if available).
| Score System | Description | Code | Codesystem |
|---|---|---|---|
1. Intensive Care and Anasthesia |
|||
| ABSI | Abbreviated burn severity index | n.v. | |
| AIS | Abbreviated Injury System | 273254002 | Snomed CT |
| APACHE | Acute Physiology And Chronic Health Evaluation Score
APACHE 2: | 9264-3 9265-0 | LOINC |
| ASA | American Society of Anesthesiologists physical status classification | 273270000 413347006 | Snomed CT |
| CASUS | Cardiac Surgery Score | tbd | |
| GCS | Glasgow Coma Scale (Beurteilung von Bewusstseinsstörungen bei Erwachsenen) | 9269-2 35088-4 386560004 | LOINC LOINC Snomed CT |
| HIS | Hannover Intensiv Score | tbd | |
| HTI | Hospital Trauma Index | 273525007 | Snomed CT |
| ISS | Injury Severity Score | 273533008 | Snomed CT |
| KISS | Kombiniertes Intensiv Scoring System | n.v. | |
| LOD | Logistic Organ Dysfunction Score | 58577001 | Snomed CT |
| MOD | Multiple Organ Dysfunction Score | ||
| MOF | Multi-Organ-Failure-Score | tbd | |
| MPI | Mannheimer Peritonitis Index | tbd | |
| Ramsay | Ramsay sedation scale | 281400004 | Snomed CT |
| RASS | Richmond Agitation Sedation Scale | n.v. | |
| SAPS | Simplified Acute Physiology Score
SAPS: 273811002 Snomed CT |
||
| SOFA | Sepsis-related Organ Failure Assessment | n.v. | |
| TI | Trauma Index | 273883005 | Snomed CT |
| TISS | Therapeutic Intervention Scoring System: TISS-10 TISS-28 TISS-76 | 273878002 tbd | Snomed CT ICD-10-GM |
| TS | Trauma Score | 273884004 | Snomed CT |
|
... |
|||
2. Patient Care |
|||
| Barthel-Index | Barthel Index | 273302005 | Snomedt CT ICD-10-GM |
| Barthel-Index, expanded | cognitive function | ICD-10-GM | |
| Braden Scale | Braden Scale | 38227-5 | LOINC |
| Braden Skin Ass. Pnl | Skin Assessment Pnl | 38228-3 | LOINC |
| BradenQ | Braden Scale for young children (<5 years) | tbd | LOINC |
| FIM | Functional Independence Measure | 273469003 U50.- | Snomed CT ICD-10-GM |
| FRB | Frührehabilitations-Barthel-Index after Schönle | U52.- 273302005 | ICD-10-GM Snomed CT |
| NEMS | Nine equivalents of nursing manpower use score | n.v. | |
| Norton | Norton score | 278898009 | Snomed CT |
| PPR | Pflegepersonal-Regelung | n.v. | |
| Waterlow | Waterlow pressure sore risk score | 278897004 | Snomed CT |
|
... |
|||
3. Psychiatry and Psychology |
|||
| AMDP | Arbeitsgemeinschaft für Methodik und Dokumentation in der Psychiatrie | n.v. | |
| LFP | Lübecker Fähigkeitenprofil | n.v. | |
| Melba | Merkmalprofile zur beruflichen Eingliederung von Behinderten | n.v. | |
| MMSE | Mini Mental State Examination | 273617000 | Snomed CT ICD-10-GM |
|
... |
|||
4. Pediatry |
|||
| Pediatric GCS | Pediatric Glasgow Coma Scale | n.v. | |
| APGAR | after 1 minute after 5 minutes |
9272-6 |
LOINC |
|
... |
|||
5. Mobility |
|||
| Tinetti-Test | |||
| Timed “Up & Go | |||
| Tandemstand | |||
| Tandemgang | |||
| Chair-Stand-Up | |||
|
... |
|||
6. Cognition |
|||
| DemTect | |||
| TFDD | Test zur Früherkennung von Demenzen mit Depressionsabgrenzung | ||
| Clock Completion | |||
|
... | |||
7. Nutrition |
|||
| MNA | Mini Nutritional Assessment(after Guigoz et.al.) | ||
|
... |
|||
8. Psychology |
|||
| APS | Acute Physiology Score | ||
9. Geriatry |
|||
| GDS | Geriatric Depression Scale | 273481004 48544-1 | Snomed CT LOINC |
10. not otherwise classified |
|||
| Bone density | 385342005 | Snomed CT | |
| BMI | Body-Mass-Index measurement Body-Mass-Index | 39156-5 41909-3 | LOINC LOINC |
| BV | Bacterial vaginosis score | B96. N76. | ICD 10 |
| FLACC | Face Legs Activity Cry Cinsolability Score | tbd | |
| Gleason | Gleason Score | 372278000 | Snomed CT |
| HTI | Hospital Traum Index | 273525007 | Snomed CT |
| IADL | IADL (after Lawton and Brody) | ||
| LBK | Lübecker Fähigkeitenprofil | ||
| MPM | MPM 2 (0) MPM 2 (24, 48, 72) Mortality Prediction Model | 273630004 273631000 | Snomed CT Snomed CT |
| PHQ | Personal Health Questionnaire (Depression Score) | ||
| PSR | Periodontal Screening and Recording | ||
| VAS | visuell analog Scala | tbd | |
|
... |
|||
Code-Systems
The code systems are identified by their OIDs which are listed in the following table.
| Codesystem | Descrption | OID | |
|---|---|---|---|
| LOINC | Logical Observation Identifiers Names and Codes | [www.loinc.org] | 2.16.840.1.113883.6.1 |
|
ICD 10 GM 2005 icd10gm2005 | ICD-Katalog (German modification 2005) | [www.dimdi.de] | 1.2.276.0.76.5.304 |
|
ICD 10 GM 2006 icd10gm2006 | ICD-Katalog (German modification 2006) | [www.dimdi.de] | 1.2.276.0.76.5.311 |
|
ICD 10 GM 2007 icd10gm2007 icd10gm2007 | ICD-Katalog (German modification 2007) | [www.dimdi.de] | 1.2.276.0.76.5.318 |
|
ICD 10 GM 2008 icd10gm2008 | ICD-Katalog (German modification 2008) | [www.dimdi.de] | 1.2.276.0.76.5.330 |
|
ICD 10 GM 2009 icd10gm2009 | ICD-Katalog (German modification 2009) | [www.dimdi.de] | |
| Snomed CT | SNOMED CT is a concept-based, scientifically validated terminology that provides a unique and permanent concept identifier that can be included in multiple HL7 data types including CD and CE. The concepts are managed to avoid "semantic drift" so the meaning remains constant. If the concept is found to be ambiguous or the meaning changes, the concept is inactivated but still retained and the identifier is never reused. SNOMED CT's concepts are interrelated hierarchically and using description logic. | [www.snomed.org] | 2.16.840.1.113883.6.96 |
|
OPS 2006 ops2006 | Operationsschlüssel | [www.dimdi.de] | 1.2.276.0.76.5.310 |
|
OPS 2007 ops2007 | Operationsschlüssel | [www.dimdi.de] | 1.2.276.0.76.5.317 |
|
OPS 2008 ops2008 | Operationsschlüssel | [www.dimdi.de] | 1.2.276.0.76.5.331 |
|
OPS 2009 ops2009 | Operationsschlüssel | [www.dimdi.de] | |
|
Alpha-ID 2008 alphaid208 | Alpha-Id 2008 | [www.dimdi.de] | 1.2.276.0.76.5.329 |
|
Alpha-ID 2009 alphaid209 | Alpha-Id 2009 | [www.dimdi.de] |
Changes from Previous Release
There is currently no previous release. Therefore, this section will be filled next cycle.
Foundation
Assessment Scales – Scores Structure Overview:
Given the interest in earlier versions of the Care Provision Ballot, further work has been undertaken on representing assessment scales, scores or indexes. The scientific testing of such instruments puts specific requirements and constraints on its use in HL7 v3 message structures in order to not only have a semantically equivalent data exchange, but also to keep the clinimetric characteristics of the instruments as a whole. The assessment scales, scoring systems or indexes are observations with specific characteristics. They can consist of severity classification systems or point totals systems that pretend to make a quantitative statement on the severity and prognosis of a disease or other aspect of human functioning. It is quite often an attempt to convert ‘soft’ observations into ‘hard’ data and evidence. Most of such instruments used in healthcare have been tested extensively on validity, reliability and usability. Many of such scoring instruments are used for decades and worldwide. Typically, assessment scales or scores combine the findings of individual values into a total score which can be interpreted more easily against a reference population. In the simplest case, it is just a single value or based on two individual values, in a complex case it can consist of several dozen values which are combined using a complex mathematical calculation or statistical technique.
This R-MIM tries to give guidelines on the representation in information models, in particular against the HL7 clinical statement pattern and the care statement R-MIM for care provision.
In addition to the information model, the appropriate use of terminology and consistency between the information model and the terminology model are crucial for safe exchange of such observations.
Care Statement extract
The R-MIM for the assessment scales – scores can be seen as an extract of Clinical and Care Statement Pattern, thus inheriting its characteristics. The R-MIM representation starts on top with the name and identification in the entry-point. For a detailed explanation of all attributes and vocabulary, the reader is referred to generic descriptions of the Reference Information Model, and to the walkthrough of the care statement D-MIM.
Score Observation
The R-MIM then starts with the score observation out of the choice box. As said above, the crucial attributes include:
- code to use a code to identify the variable and in which also the code system can be listed.
- text attribute to allow the name and description of the assessment instrument
- value in which the actual score and where applicable the unit can be entered
- interpretationCode where the interpretation of the value can be explained via codes, often against a reference value In the derivation code the total score for the assessment scale is recorded. In other words: derivation method is for example to add all values of the separate scores towards the total score.
- Effective time is the point in time on which the instrument is scored. In order to be valid and reliable, the scoreItems need to have (almost) the same time stamp. Such constraints posed by assessment instruments are important and expand beyond the mere semantic interoperability. For the receiver it is not only important to understand what the message content means, but also be ascertained that the data are collected based on the guidelines for the instrument.
- In the value of the score, which was created by adding the individual score items, is filled up. This is often a Coded Ordinal data type because it is mandatory to score and fill up all items to get a proper sum score. That is why Mandatory (1..1) component relations often exist for scoring instruments.
- Of course all relevant attributes can be applied as needed
Component relationship to ScoreItem Observation
From that point onwards a recursion starts based on the component relationship, allowing either including other score values or observations a score is based upon. Beneath the score Observation is the Observation (OBS) with the name Score item. Both the class Score and the class ScoreItem have class code = OBS.
Derived from relationship to Care Statement CMET
The derived from relation to care statement allows the user to describe any relevant information related to why a score item is scored this way. It allows to express any human thoughts as observations to go alongside with the score itself, or any circumstances as a procedure being carried out, or a specific encounter when it was measured. The relationship is to the choice box, allowing to make such statements on the level of the assessment instrument as a whole, or for an individual scoreItem.
Linkages to subject and provider roles
<to be completed>
Score System Categories
The score systems can be divided into different categories: Those with arbitrary scores, those with discrete values and those with an unspecified number of values. Patient Classification Systems for workload are examples of the first one, the Barthel index is an example of the second category, the BMI (Body Mass Index) and example for the third.
Arbitrary scores
A scale is a set of linear values from a certain range. A reference range can be determined. In this case, an interpretation according to the conventional scheme is possible, i.e. a value is interpreted as "normal" if it is within the area:
However, it should be noted here that an interpretation as too low is not necessarily combined with the abnormal flag.
Discrete values (scores)
The normal range and the number of all possible values are identical. So for example, the Barthel Index allows for the values of 0 to 100 in steps of 5. The reference range, which can be specified, is within the same range, so that the available assessment opportunities (Abnormal flags) are not usable. The interpretation of a score is depending on a part of the reference range to which it belongs. Hence, the referenceRange relationship to another OBS with the name ScoreRange.
For example:
Interpretation shows how the total score should be interpreted. For instance for the Dutch version of the Barthel index, this is 0-9 for seriously limited, 10-19 for moderately limited and 20 for independent. Finally the ScoreChoice box has participations with subject and author as explained in detail in the clinical statement pattern. As mentioned above, an assessment of the results by the conventional scheme of a reference range, where values outside are too high or too low, does not to apply. All values are falling into the range as defined by the score system. This range is - as explained above - to be divided into sections, which then can be evaluated/interpreted separately. Each score system is going to have its own (new) set of interpretation values. Each score system should get its own set of interpretation values which can be defined according to the following scheme. If the code values are coming from different code systems, then they must be included:
Table : Interpretation of results Eventually, some score systems may share the same interpretations.
Storyboard
This D-MIM can be used in different circumstances. Right now, four different use cases are foreseen.
Assessment Scale Define
The D-MIM can be used in definition mood, so that it can convey information about the score system resp. assessment scale itself.
Assessment Scale Order
The primary codes, i.e. the ones on top level and not for the components, can be used to send a request for an observation using scores and assessments.
Assessment Scale Observation
The result of such an observation can be transmitted.
Assessment Scale Query
It should be possible to query for previous results as well.
Application Roles
According to the use case different combinations of application roles are applicable:
- informer - tracker
- placer - fulfiller
- query placer - query fulfiller
Trigger Events
The associated trigger events depend on the use case. This template an be used in messages and/or documents. Therefore, the events will vary.
Refined Message Information Models
HL7 V3 provides the "Clinical Statement Pattern". Here one can find the activity "Observation" with the necessary details. Facilitating this "basic structure", the pattern/template can be reused in other domains as well.
A_ObservationAssessmentScales-Scores (REPC_RM000125UV)
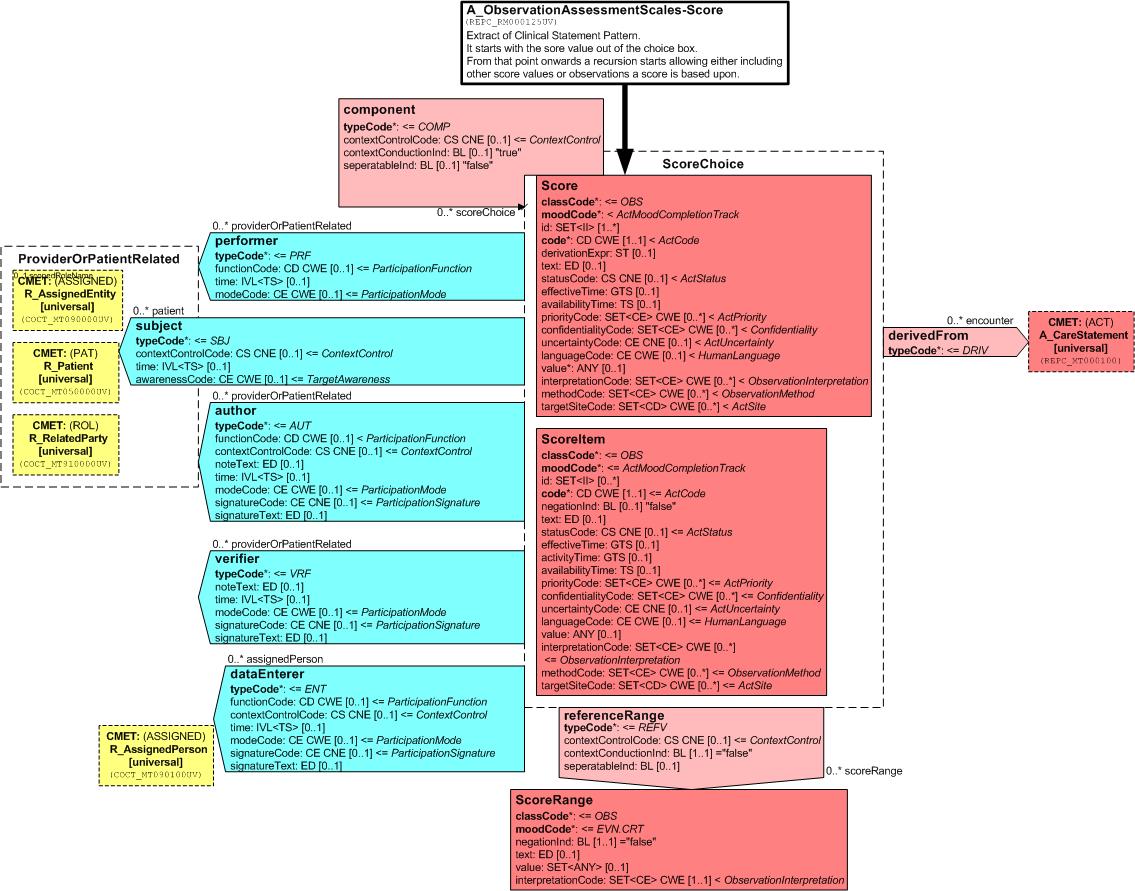
A score or assessment value is an observation. Therefore, as an entry point the observation act has been chosen. If the total score value is to be transferred only, they may use the Observation-Act directly (and exclusively).
But if the total score including all individual observations, the latter has to be assigned to the score as components. This assignement is done recursively so that a component can be a score itself. Within this recursion one can refer to a score or an observation which is used to calculate the total score. Therefore, the act relationship link is done from Score to ScoreChoice.
Both classes can be linked by participations to CMETs for performer, verifier, author etc. or to refer to a reference range.
Walkthrough
The walkthrough will be done in the following order:
- Score
- Score Item
- Act-Relationship component
- Participation author
- Participation unterzeichzner
- Participation verifier
- Participation performer
- Participation dataEnterer
- Participation subject
- Act-Relationship referenceRange
- Score Range
Class Score
This act conveys information about the score itself and acts as a container (grouping) for the details to this score.
classCode := OBS
A score is an observation. Therefore the classCode is set to “OBS”.
moodCode <= ActMoodCompletionTrack
This value can come from ActMoodCompletionTrack and therefore allows to use in different business cycles. Normally, using "EVN" is foreseen. But "RQO" for requests or "DEF" for conveying information about itself is permitted as well.
Here we have to admit, that "DEF" is officially not allowed within clinical statement patterns. This is an action item for the next harmonization meeting.
id (Score-ID) := SET<II> [1..*]
Each Score is identified by a unique id. A value must be provided, esp. if the information is used in different phases of a business cycle.
code (score system) := CD CWE [1..1]
This is the primary value to identify the score system and therefore mandatory. The value may come from different code systems. The possible values can be found in the database.
derivationExpr (calculation method) := ST [0..1]
This optional field can be used to specify how the total score is calculated. In most cases to total score will be the sum of its components. But complex mathematical functions are possible as well. In some cases the calculation is a matter of copyright issues.
| function | description | Example |
|---|---|---|
| direct value | Score only consists of a single value. This vlaue is just interpreted. | RASS Ramsay |
| sum | The different details are single values which are added into a total. | Barthel Apache II |
| mathematical calculation | The details are combined according to a mathematical functions. | BMI |
| combination | The values are combined somehow, e.g. by concatenation. | PPR |
|
... | ||
statusCode (Status) := CS CNE [1..1] <= ActStatus
In most cases the information is transmitted after calculation. Therefore, the statusCode will be "completed".
effectiveTime (observation time) := GTS [0..1]
availabilityTime := TS [0..1]
priorityCode := SET<CE> CWE [0..*] <= ActPriority
confidentialityCode := SET<CE> CWE [0..*] <= Confidentiality
uncertaintyCode := CE CNE [0..1] <= ActUncertainty
languageCode (language) := CE CWE [0..1] <= HumanLanguage
value (total Score Value) := ANY [0..1]
This field contains the value of the total score itself. Normally, it will be an integer or coded ordinal. But other datatypes like strings as for PPR ("A1S2") or real values for BMI are allowed as well.
interpretationCode (Interpretation) := SET<CE> CWE [0..*] <= ObservationInterpretation
This field contains the interpretationof the score value. The code comes from a value set which has been defined for this score system.
methodCode := SET<CE> CWE [0..*] <= ObservationMethod
targetSiteCode := SET<CD> CWE [0..*] <= ActSite
Class ScoreItem
Like the class Score this act conveys information about the component to a score.
classCode := OBS
This act is a placeholder for individual observations. Therefore the classCode is set to “OBS”.
moodCode <= ActMoodCompletionTrack
This value can come from ActMoodCompletionTrack and therefore allows to use in different business cycles. Normally, using "EVN" is foreseen.
id (Score-ID) := SET<II> [0..*]
Each component can be identified by a unique id. A value can be provided, esp. if the information is used in different phases of a business cycle.
code (score system) := CD CWE [1..1] <= ActCode
This is the primary value to identify the component of the score system and is therefore mandatory. The value may come from different code systems. The possible values can be found in the database.
negationInd := BL [0..1]
text := ED [0..1]
statusCode (status) := CS CNE [1..1] <= ActStatus
In most cases the information is transmitted after calculation. Therefore, the statusCode will be "completed".
effectiveTime (observation time) := GTS [0..1]
availabilityTime := TS [0..1]
priorityCode := SET<CE> CWE [0..*] <= ActPriority
confidentialityCode := SET<CE> CWE [0..*] <= Confidentiality
uncertaintyCode := CE CNE [0..1] <= ActUncertainty
languageCode (language) := CE CWE [0..1] <= HumanLanguage
value (score value) := ANY [0..1]
This field contains the value of the score component.
interpretationCode (interpretation of the value) := SET<CE> CWE [0..*] <= ObservationInterpretation
This field contains the interpretation of the score component value. The code comes from a value set which has been defined for this component of the score system.
methodCode := SET<CE> CWE [0..*] <= ObservationMethod
targetSiteCode := SET<CD> CWE [0..*] <= ActSite
Act-Relationship component
This act relationship is used to link a score (as parent) to its components (as children). The use is optional.
typeCode := COMP
Diese Angabe verweist auf die Einzelinformationen, aus denen sich der Score-Wert zusammensetzt.
Participation performer
s. VHitG-Arztbrief
typeCode <= PRF
Participation author
Using this participation the information about the author is included.
author (Angaben zum Author) := [0..*]
Optional können die Score-Werte mit anderen Authorangaben versehen werden.
typeCode <= AUT
functionCode (function of the author) := CE CWE [1..1] <= ParticipationFunction
In der verpflichtenden Funktionsangabe wird angegeben, in welcher Funktion der Author an der Erstellung der Score-Werte mitgewirkt hat.
contextControlCode := CS CNE [0..1] <= ContextControl
noteText := ED [0..1]
time (Zeitpunkt der Dokumentation) := TS [1..1]
Im verpflichtend anzugebenden time Attribut wird der Zeitpunkt der Dokumentation angegeben.
modeCode := CE CWE [0..1]
signatureCode := CE CNE [0..1] <= ParticipationSignature
signatureText := ED [0..1]
Participation Unterzeichner
Ähnlich dem Author können diverse Unterzeichner angefügt werden. Diese Participation ist in obiger Grafik übersichtshalber nicht enthalten.
Participation verifier
s. VHitG-Arztbrief
typeCode <= VRF
Participation dataEnterer
This participation is linked to the R_AssignedPerson CMET.
typeCode <= ENT
Participation subject
Using this participation information about the patient is conveyed. This participation is linked to the R_Patient CMET.
typeCode <= SBJ
contextControlCode := CS CNE [0..1] <= ContextControl
time (Zeitpunkt der Dokumentation) := TS [1..1]
awarenessCode := CE CWE [0..1] <= TargetAwareness
CMET Choice Box
The following CMETs are assigned to the previously listed participations:
- R_AssignedEntity [universal]
- R_Patient [universal]
- R_RelatedParty [universal]
- R_AssignedPerson [universal]
Act-Relationship referenceRange
Über diese (optionale) Beziehung wird der Referenzbereich für den Score-Wert festgelegt. Das ist der Bereich der Werte, in dem die meisten (aber nicht alle) Gesunden liegen sollten.
Mitunter gelten die Bereichsfestlegungen über Normalwerte nicht, da die gemessenen/errechneten Werte alle innerhalb des Normbereiches liegen, jedoch unterschiedlich interpretiert werden müssen. In diesem Fall findet die „Precondition“ Anwendung.
typeCode := REFV
Diese Angabe deklariert die Beziehung als Bereichsfestlegung.
contextControlCode := CS CNE [0..1] <= ContextControl
contextConductionInd := BL [1..1] = "false"
seperatableInd := BL [0..1]
Diese Information gibt an, ob die Quell-Klasse (Score-Wert) auch ohne den Referenzbereich genutzt werden darf oder nicht.
class ScoreRange
In dieser Klasse werden die Normbereiche – evtl. mit Vorbedingungen – übermittelt.
classCode := OBS
Da es sich hier ebenfalls um eine Beobachtung handelt ist der classCode natürlich “OBS”.
moodCode := EVN.CRT
Die Einzelwerte als Grundlage des Score-Wertes sind ermittelt worden, d.h. sie liegen vor und werden deshalb im Event-Mood übermittelt.
negationInd := Verneinung BL [1..1] <= false
Die Normbereiche werden nicht verneint.
text := ED [0..1]
value (Bereichswert) := ANY CWE [1..1] =
In diesem Feld wird der Normwertbereich angegeben. Typischerweise wird er als Intervall kommuniziert. Es ist aber auch denkbar, dass hier eine Wertemenge angegeben wird, so dass der Datentyp SET<T> zum Einsatz kommt.
interpretationCode := CE CWE [1..1] <= ObservationInterpretation
Hierarchical Message Descriptions
tbd
Dynamic Model
This information model represents a generic template which can be used in messages and documents as well.
Open Issues
Description Parent: Care Structures Event Statement (REPC_RM000100UV)