Difference between revisions of "201801 Care Plan"
| (50 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
| __TOC__ | | __TOC__ | ||
|} | |} | ||
| − | =Care | + | =Care Management and Planning= |
| − | '''Dedicated [https://chat.fhir.org/#narrow/stream/connectathon.20mgmt/subject/ | + | '''Dedicated [https://chat.fhir.org/#narrow/stream/connectathon.20mgmt/subject/Care.20Management.20and.20Planning Zulip chat stream] for this track.''' |
| − | + | '''Connectathon Orientation and Track Overview''' | |
| − | + | * Presentation slides [http://wiki.hl7.org/images/a/a6/FHIR_Connectathon_Track_Orientation_-_Care_Management.pptx as PowerPoint] | |
| − | * [http:// | + | |
| + | '''Summary presentation slides after conclusion of Care Management track''' | ||
| + | * See Outcomes section below | ||
| + | * Presentation slides TBD | ||
'''Previous Care Plan Connectathons''' | '''Previous Care Plan Connectathons''' | ||
| Line 17: | Line 20: | ||
* [[201701 Care Plan]], January 2017, San Antonio, TX | * [[201701 Care Plan]], January 2017, San Antonio, TX | ||
| − | + | ==Submitting WG/Project/Implementer Group== | |
| − | * | + | * [[Patient_Care | HL7 Patient Care Workgroup]] |
| + | * [http://hspconsortium.org Healthcare Services Platform Consortium (HSPC)] | ||
| + | * Allscripts | ||
==Justification== | ==Justification== | ||
<!--Why is this an important track to include in the connectathon - include implementer need, impact on ballot, FMM readiness of the resources, etc. --> | <!--Why is this an important track to include in the connectathon - include implementer need, impact on ballot, FMM readiness of the resources, etc. --> | ||
| − | This track is intended to advance the maturity of FHIR resources for care | + | This track is intended to advance the maturity of FHIR resources for care management ([http://hl7.org/fhir/careplan.html CarePlan], [http://hl7.org/fhir/careteam.html CareTeam], [http://hl7.org/fhir/goal.html Goal], [http://hl7.org/fhir/condition.html Condition], and others), the definition of computable clinical protocols ([http://hl7.org/fhir/plandefinition.html PlanDefinition], [http://hl7.org/fhir/activitydefinition.html ActivityDefinition]), and to document industry best practices for improving care coordination using shared care plans. This work will inform the development of more comprehensive implementation guides and profiles for care management based on FHIR Release 3 (STU), which is the primary target for testing in this track. This connectathon track will be coordinated with the Chronic Conditions track at [http://wiki.hl7.org/index.php?title=Clinicians_on_FHIR_-_Jan_2018,_New_Orleans._LA Clinicians on FHIR] where they focus on ''clinical interoperability'' and harmonizing differences between the technical and clinical perspectives of FHIR resources. |
| − | + | In addition to advancing the maturity of FHIR resources for care management, this track invites participation by clinicians and implementers who are interested in ''using'' these FHIR standards to realize the benefits of comprehensive shared care management coordinated across provider organizations. Two participant roles are included (Care Plan Protocol Creator & CDS Service Requestor) that engage the practitioner community to evaluate and demonstrate use of FHIR care management resources for the active management of a patient's healthcare. | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | In addition to advancing the maturity of FHIR resources for care | ||
==Proposed Track Lead== | ==Proposed Track Lead== | ||
| − | :Dave Carlson – | + | :Dave Carlson – VHA |
::E-mail: dcarlson@ClinicalCloud.solutions | ::E-mail: dcarlson@ClinicalCloud.solutions | ||
::Zulip: Dave Carlson | ::Zulip: Dave Carlson | ||
| Line 40: | Line 39: | ||
The following organizations have indicated an interest in participating in this track: | The following organizations have indicated an interest in participating in this track: | ||
| − | |||
| − | |||
* Allscripts | * Allscripts | ||
| + | * Cerner | ||
| + | * Clinical Cloud Solutions | ||
| + | * Healthcare Services Platform Consortium (HSPC) | ||
* InterSystems | * InterSystems | ||
| + | * Veterans Health Administration (VHA) | ||
| + | * Zynx Health | ||
* ''Your organization here!'' | * ''Your organization here!'' | ||
| Line 50: | Line 52: | ||
===Care Plan Server=== | ===Care Plan Server=== | ||
| − | A FHIR server (version 3.0) should support the following resources for this | + | A FHIR server (version 3.0) should support the following resources for this role: |
| − | * CarePlan, | + | * CarePlan, Condition, Goal, CareTeam, and other resources referenced by CarePlan.activity.reference |
| − | |||
A FHIR server is available for testing with sample data that represent one or more care plan scenarios. | A FHIR server is available for testing with sample data that represent one or more care plan scenarios. | ||
* HSPC sandbox server (FHIR 3.0.1) at https://api-stu3.hspconsortium.org/careplantest/open | * HSPC sandbox server (FHIR 3.0.1) at https://api-stu3.hspconsortium.org/careplantest/open | ||
| − | * Test data JSON files are [https://github.com/clinical-cloud/sample-data available in a GitHub repository] that may be loaded into other FHIR v3.0 servers. | + | * Test data JSON files with several patient care plans are [https://github.com/clinical-cloud/sample-data available in a GitHub repository] that may be loaded into other FHIR v3.0 servers. |
===Care Plan Requestor=== | ===Care Plan Requestor=== | ||
| − | |||
This connectathon track imposes few requirements for interested participants to evaluate and test retrieval of care plan resources from a Care Plan Server. We wish to encourage discussion and testing that will lead to robust industry support for shared care plans. Thus, a requestor role could be fulfilled by a range of applications, such as the following: | This connectathon track imposes few requirements for interested participants to evaluate and test retrieval of care plan resources from a Care Plan Server. We wish to encourage discussion and testing that will lead to robust industry support for shared care plans. Thus, a requestor role could be fulfilled by a range of applications, such as the following: | ||
* Debug testing tools for RESTful services, e.g. Postman, that allow query of participating Care Plan Server using a variety of parameters such as plan category or date. | * Debug testing tools for RESTful services, e.g. Postman, that allow query of participating Care Plan Server using a variety of parameters such as plan category or date. | ||
* SMART on FHIR applications that embed Care Plan review and editing capabilities into any EHR system that supports these services. | * SMART on FHIR applications that embed Care Plan review and editing capabilities into any EHR system that supports these services. | ||
| − | * SMART on FHIR mobile applications that enable patients to view, contribute to, or | + | * SMART on FHIR mobile applications that enable patients to view, contribute to, or complete activities included in a care plan created by their care team member(s). |
| + | |||
| + | ===Care Plan Protocol Creator=== | ||
| + | A FHIR server (version 3.0) should support the following resources for this role: | ||
| + | * [http://hl7.org/fhir/plandefinition.html PlanDefinition] and [http://hl7.org/fhir/activitydefinition.html ActivityDefinition] | ||
| + | ** Bonus points for using CQL in conditional logic expressions for plan activities | ||
| + | |||
| + | * Create and share care protocol definitions via FHIR server endpoint | ||
| + | ** Care guidelines, e.g. for new diabetes diagnosis, or managing the progression of chronic kidney disease | ||
| + | ** Order set definitions that recommend modification of activities in existing care plans, e.g. modify medications based on vital sign or lab observation feedback; see CDS integration | ||
===CDS Service Requestor=== | ===CDS Service Requestor=== | ||
| − | * [[ | + | * Coordinate with [[201801_CDS_Hooks]] track |
* Invoke a [http://cds-hooks.org/ CDS Hooks Service] that guides a clinician or a patient toward fulfillment of a Care Plan's goals, or suggests additional activities based on clinical practice guidelines. The CDS Hooks Service provides real-time clinical decision support as a remote service, where the CDS Server is invoked on a desired hook and returns the decision support in the form of CDS cards. | * Invoke a [http://cds-hooks.org/ CDS Hooks Service] that guides a clinician or a patient toward fulfillment of a Care Plan's goals, or suggests additional activities based on clinical practice guidelines. The CDS Hooks Service provides real-time clinical decision support as a remote service, where the CDS Server is invoked on a desired hook and returns the decision support in the form of CDS cards. | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==Scenarios== | ==Scenarios== | ||
| − | This track emphasizes dynamic care | + | This track emphasizes dynamic care management scenarios where one or more care plans are created, accessed, or updated by one or more members of the care team during the provision of healthcare, and the care plans are used by a patient or his/her caregivers to review or perform plan activities. These scenarios illustrate communication flow of care plan(s) between a patient, his or her primary care provider, consulted specialists, home health care, telehealth care, and family caregivers involved in management of care for one or more health conditions. |
| − | ===Chronic | + | ===Chronic Care Management=== |
| − | + | Our recommended clinical use case is based on the [https://www.niddk.nih.gov/health-information/communication-programs/nkdep/working-groups/health-information-technology/development-electronic-ckd-care-plan NIH Chronic Kidney Disease (CKD) Care Plan project]. Because frequent transitions of care are common among patients with CKD, an electronic CKD care plan could potentially improve patient outcomes by helping to ensure that critical patient data are consistently available to both the patient and his/her providers. | |
| − | * | + | * Persona descriptions for patients with CKD and their provider care team members are available from the NIH site: |
| − | ** | + | ** [https://www.niddk.nih.gov/-/media/Files/Health-Information/Communication-Programs/NKDEP/Patient_Personas_508.pdf?la=en Patient personas]; this track's sample data are based on Betsy Johnson's persona |
| − | * | + | ** [https://www.niddk.nih.gov/-/media/Files/Health-Information/Communication-Programs/NKDEP/Provider_Personas_508.pdf?la=en Provider personas] for six members of a CKD patient's care team |
| − | * | + | * A draft set of data elements and terminology codes are also available for CKD care management, created by the NIH CKD Care Plan Working Group |
| − | ** | + | ** [https://www.niddk.nih.gov/health-information/communication-programs/nkdep/working-groups/health-information-technology/development-electronic-ckd-care-plan#draftSet CKD Data Elements] |
| − | * | + | * Example FHIR resource data were created for testing, based on these CKD patient and provider personas and data elements |
| − | ** | + | ** JSON sample FHIR resource files for patient persona Betsy Johnson (contributions welcome!). See https://github.com/clinical-cloud/sample-data/chronic-conditions |
| − | ** | + | ** These sample data are also loaded into this track's HSPC sandbox FHIR server, https://api-stu3.hspconsortium.org/careplantest/open |
| − | |||
| − | === | + | ===Scenario 1: Retrieve a patient's care plan(s)=== |
| + | Search for a patient's care plans(s) and associated resources (Conditions, Goals, activity references, CareTeam) | ||
| + | * An end-user client application enables patients and/or care team members to search for and view care plans and their referenced resources. | ||
| + | * A server-based application queries a patient's care plans and other clinical resources | ||
| + | ** e.g. a population health or analytics product vendor retrieves a patient's care plans and related resources for aggregation, analysis, and sharing with other care team members | ||
| + | * Bonus points for demonstrating SMART on FHIR applications or other use of OAuth security that authorizes access to patient data | ||
| − | + | ===Scenario 2: Create new care plan from protocol definition=== | |
| − | + | * Generate a [http://hl7.org/fhir/careplan.html CarePlan] from a [http://hl7.org/fhir/plandefinition.html PlanDefinition] protocol, customized using the current [http://hl7.org/fhir/patient.html Patient]'s context | |
| − | * | + | ** Use PlanDefinition [http://hl7.org/fhir/plandefinition-operations.html#apply $apply operation] |
| − | + | ** Save the resulting CarePlan resource on a FHIR server, making it available to participants of the other track roles and scenarios | |
| − | |||
| − | * | ||
| − | == | + | ===Scenario 3: Request CDS 'patient-view' hook=== |
| − | + | * Invoke 'patient-view' hook on one or more CDS Hook service providers | |
| + | * Display returned cards | ||
| + | ** Cards may include any combination of information (for reading), suggested actions (to be applied if a user selects them), and links (to launch an app if the user selects them). The client application decides how to display cards, but CDS Hooks specification recommends displaying suggestions using buttons, and links using underlined text. | ||
| − | + | Example clinical scenarios for integrating CDS: | |
| − | + | * Evaluate progress toward care plan goals | |
| + | ** Query and analyze relevant Observations related to a Goal target measure (e.g. blood glucose, weight, etc.) | ||
| + | ** Return CDS Hook cards notifying care team members about lack of progress on goal targets | ||
| + | * Recommend additions to care plan activities based on current Patient status or revised diagnoses | ||
| + | ** Return CDS Hook cards with information or suggestions based on clinical practice guidelines for chronic condition management | ||
| − | + | ==Outcomes== | |
| − | + | ===Goal=== | |
| − | + | Advance the maturity of FHIR resources for care management ([http://hl7.org/fhir/careplan.html CarePlan], [http://hl7.org/fhir/careteam.html CareTeam], [http://hl7.org/fhir/goal.html Goal], [http://hl7.org/fhir/condition.html Condition], and others), the definition of computable clinical protocols ([http://hl7.org/fhir/plandefinition.html PlanDefinition], [http://hl7.org/fhir/activitydefinition.html ActivityDefinition]), and to document industry best practices for improving care coordination using shared care plans. This work will inform the development of more comprehensive implementation guides and profiles for care management based on FHIR Release 3 (STU), which is the primary target for testing in this track. This connectathon track will be coordinated with the Chronic Conditions track at [http://wiki.hl7.org/index.php?title=Clinicians_on_FHIR_-_Jan_2018,_New_Orleans._LA Clinicians on FHIR] where they focus on ''clinical interoperability'' and harmonizing differences between the technical and clinical perspectives of FHIR resources. | |
| − | + | ===Participants=== | |
| − | + | * Academy of Nutrition and Dietetics | |
| − | + | * Allscripts | |
| + | * Cerner | ||
| + | * Clinical Cloud Solutions | ||
| + | * Healthcare Services Platform Consortium (HSPC) | ||
| + | * InterSystems | ||
| + | * Lantana Consulting Group | ||
| + | * SAMHSA | ||
| + | * Veterans Health Administration (VHA) | ||
| − | === | + | ===Notable Achievements=== |
| − | + | * Successful collaboration with clinical use case based on the [https://www.niddk.nih.gov/health-information/communication-programs/nkdep/working-groups/health-information-technology/development-electronic-ckd-care-plan NIH Chronic Kidney Disease (CKD) Care Plan project]. Because frequent transitions of care are common among patients with CKD, an electronic CKD care plan could potentially improve patient outcomes by helping to ensure that critical patient data are consistently available to both the patient and his/her providers. | |
| + | * Successful results associating PlanDefinitions with applicable ActivityDefinition for a Diabetes care protocol and creating a recommended CarePlan for a specific patient. | ||
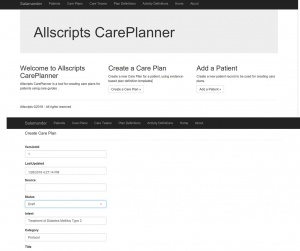
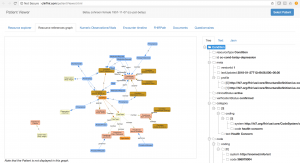
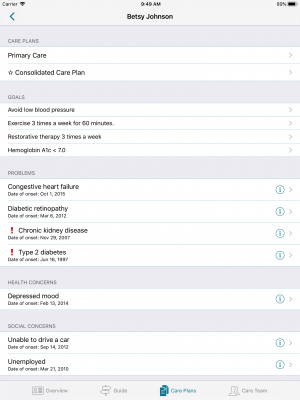
| + | ===Screenshots=== | ||
| + | [[Image:Care Plans using planDefinition.jpg|300px]] | ||
| + | [[Image:CarePlan-clinFHIR-CKD.png|300px]] | ||
| + | [[Image:CKD-patient-iPad-app.png|300px]] | ||
| − | + | ===Discovered issues=== | |
| − | * | + | * Questions on use of clinFHIR to create and edit example FHIR resources for the CKD use case using a shared HSPC FHIR server. Successful and happy users after scheduling a breakout room review with David Hay. |
| − | + | *What questions did you come away with? | |
| − | * | + | ===Next Steps=== |
| − | + | * Illustrate benefits and use of distributing a library of care protocols using FHIR PlanDefinition, and applying those protocols to improve care management / care coordination by using: | |
| − | + | ** CDS to create or update patient care plans | |
| − | * | + | ** Provider directories to improve care coordination |
| − | ** | + | * Support use of evidence-based protocols for care planning with FHIR PlanDefinitions |
| − | * | + | * Continue to expand comprehensive FHIR care planning example for Chronic Kidney Disease and other conditions |
| − | * | + | ** Document best practices and FHIR implementation guides for care managment |
| − | * | ||
Latest revision as of 15:51, 29 January 2018
Care Management and Planning
Dedicated Zulip chat stream for this track.
Connectathon Orientation and Track Overview
- Presentation slides as PowerPoint
Summary presentation slides after conclusion of Care Management track
- See Outcomes section below
- Presentation slides TBD
Previous Care Plan Connectathons
- 201709 Care Plan, September 2017, San Diego, CA
- 201704 Care Plan, April 2017, Chicago, IL
- 201701 Care Plan, January 2017, San Antonio, TX
Submitting WG/Project/Implementer Group
Justification
This track is intended to advance the maturity of FHIR resources for care management (CarePlan, CareTeam, Goal, Condition, and others), the definition of computable clinical protocols (PlanDefinition, ActivityDefinition), and to document industry best practices for improving care coordination using shared care plans. This work will inform the development of more comprehensive implementation guides and profiles for care management based on FHIR Release 3 (STU), which is the primary target for testing in this track. This connectathon track will be coordinated with the Chronic Conditions track at Clinicians on FHIR where they focus on clinical interoperability and harmonizing differences between the technical and clinical perspectives of FHIR resources.
In addition to advancing the maturity of FHIR resources for care management, this track invites participation by clinicians and implementers who are interested in using these FHIR standards to realize the benefits of comprehensive shared care management coordinated across provider organizations. Two participant roles are included (Care Plan Protocol Creator & CDS Service Requestor) that engage the practitioner community to evaluate and demonstrate use of FHIR care management resources for the active management of a patient's healthcare.
Proposed Track Lead
- Dave Carlson – VHA
- E-mail: dcarlson@ClinicalCloud.solutions
- Zulip: Dave Carlson
Expected participants
The following organizations have indicated an interest in participating in this track:
- Allscripts
- Cerner
- Clinical Cloud Solutions
- Healthcare Services Platform Consortium (HSPC)
- InterSystems
- Veterans Health Administration (VHA)
- Zynx Health
- Your organization here!
Roles
Care Plan Server
A FHIR server (version 3.0) should support the following resources for this role:
- CarePlan, Condition, Goal, CareTeam, and other resources referenced by CarePlan.activity.reference
A FHIR server is available for testing with sample data that represent one or more care plan scenarios.
- HSPC sandbox server (FHIR 3.0.1) at https://api-stu3.hspconsortium.org/careplantest/open
- Test data JSON files with several patient care plans are available in a GitHub repository that may be loaded into other FHIR v3.0 servers.
Care Plan Requestor
This connectathon track imposes few requirements for interested participants to evaluate and test retrieval of care plan resources from a Care Plan Server. We wish to encourage discussion and testing that will lead to robust industry support for shared care plans. Thus, a requestor role could be fulfilled by a range of applications, such as the following:
- Debug testing tools for RESTful services, e.g. Postman, that allow query of participating Care Plan Server using a variety of parameters such as plan category or date.
- SMART on FHIR applications that embed Care Plan review and editing capabilities into any EHR system that supports these services.
- SMART on FHIR mobile applications that enable patients to view, contribute to, or complete activities included in a care plan created by their care team member(s).
Care Plan Protocol Creator
A FHIR server (version 3.0) should support the following resources for this role:
- PlanDefinition and ActivityDefinition
- Bonus points for using CQL in conditional logic expressions for plan activities
- Create and share care protocol definitions via FHIR server endpoint
- Care guidelines, e.g. for new diabetes diagnosis, or managing the progression of chronic kidney disease
- Order set definitions that recommend modification of activities in existing care plans, e.g. modify medications based on vital sign or lab observation feedback; see CDS integration
CDS Service Requestor
- Coordinate with 201801_CDS_Hooks track
- Invoke a CDS Hooks Service that guides a clinician or a patient toward fulfillment of a Care Plan's goals, or suggests additional activities based on clinical practice guidelines. The CDS Hooks Service provides real-time clinical decision support as a remote service, where the CDS Server is invoked on a desired hook and returns the decision support in the form of CDS cards.
Scenarios
This track emphasizes dynamic care management scenarios where one or more care plans are created, accessed, or updated by one or more members of the care team during the provision of healthcare, and the care plans are used by a patient or his/her caregivers to review or perform plan activities. These scenarios illustrate communication flow of care plan(s) between a patient, his or her primary care provider, consulted specialists, home health care, telehealth care, and family caregivers involved in management of care for one or more health conditions.
Chronic Care Management
Our recommended clinical use case is based on the NIH Chronic Kidney Disease (CKD) Care Plan project. Because frequent transitions of care are common among patients with CKD, an electronic CKD care plan could potentially improve patient outcomes by helping to ensure that critical patient data are consistently available to both the patient and his/her providers.
- Persona descriptions for patients with CKD and their provider care team members are available from the NIH site:
- Patient personas; this track's sample data are based on Betsy Johnson's persona
- Provider personas for six members of a CKD patient's care team
- A draft set of data elements and terminology codes are also available for CKD care management, created by the NIH CKD Care Plan Working Group
- Example FHIR resource data were created for testing, based on these CKD patient and provider personas and data elements
- JSON sample FHIR resource files for patient persona Betsy Johnson (contributions welcome!). See https://github.com/clinical-cloud/sample-data/chronic-conditions
- These sample data are also loaded into this track's HSPC sandbox FHIR server, https://api-stu3.hspconsortium.org/careplantest/open
Scenario 1: Retrieve a patient's care plan(s)
Search for a patient's care plans(s) and associated resources (Conditions, Goals, activity references, CareTeam)
- An end-user client application enables patients and/or care team members to search for and view care plans and their referenced resources.
- A server-based application queries a patient's care plans and other clinical resources
- e.g. a population health or analytics product vendor retrieves a patient's care plans and related resources for aggregation, analysis, and sharing with other care team members
- Bonus points for demonstrating SMART on FHIR applications or other use of OAuth security that authorizes access to patient data
Scenario 2: Create new care plan from protocol definition
- Generate a CarePlan from a PlanDefinition protocol, customized using the current Patient's context
- Use PlanDefinition $apply operation
- Save the resulting CarePlan resource on a FHIR server, making it available to participants of the other track roles and scenarios
Scenario 3: Request CDS 'patient-view' hook
- Invoke 'patient-view' hook on one or more CDS Hook service providers
- Display returned cards
- Cards may include any combination of information (for reading), suggested actions (to be applied if a user selects them), and links (to launch an app if the user selects them). The client application decides how to display cards, but CDS Hooks specification recommends displaying suggestions using buttons, and links using underlined text.
Example clinical scenarios for integrating CDS:
- Evaluate progress toward care plan goals
- Query and analyze relevant Observations related to a Goal target measure (e.g. blood glucose, weight, etc.)
- Return CDS Hook cards notifying care team members about lack of progress on goal targets
- Recommend additions to care plan activities based on current Patient status or revised diagnoses
- Return CDS Hook cards with information or suggestions based on clinical practice guidelines for chronic condition management
Outcomes
Goal
Advance the maturity of FHIR resources for care management (CarePlan, CareTeam, Goal, Condition, and others), the definition of computable clinical protocols (PlanDefinition, ActivityDefinition), and to document industry best practices for improving care coordination using shared care plans. This work will inform the development of more comprehensive implementation guides and profiles for care management based on FHIR Release 3 (STU), which is the primary target for testing in this track. This connectathon track will be coordinated with the Chronic Conditions track at Clinicians on FHIR where they focus on clinical interoperability and harmonizing differences between the technical and clinical perspectives of FHIR resources.
Participants
- Academy of Nutrition and Dietetics
- Allscripts
- Cerner
- Clinical Cloud Solutions
- Healthcare Services Platform Consortium (HSPC)
- InterSystems
- Lantana Consulting Group
- SAMHSA
- Veterans Health Administration (VHA)
Notable Achievements
- Successful collaboration with clinical use case based on the NIH Chronic Kidney Disease (CKD) Care Plan project. Because frequent transitions of care are common among patients with CKD, an electronic CKD care plan could potentially improve patient outcomes by helping to ensure that critical patient data are consistently available to both the patient and his/her providers.
- Successful results associating PlanDefinitions with applicable ActivityDefinition for a Diabetes care protocol and creating a recommended CarePlan for a specific patient.
Screenshots
Discovered issues
- Questions on use of clinFHIR to create and edit example FHIR resources for the CKD use case using a shared HSPC FHIR server. Successful and happy users after scheduling a breakout room review with David Hay.
- What questions did you come away with?
Next Steps
- Illustrate benefits and use of distributing a library of care protocols using FHIR PlanDefinition, and applying those protocols to improve care management / care coordination by using:
- CDS to create or update patient care plans
- Provider directories to improve care coordination
- Support use of evidence-based protocols for care planning with FHIR PlanDefinitions
- Continue to expand comprehensive FHIR care planning example for Chronic Kidney Disease and other conditions
- Document best practices and FHIR implementation guides for care managment