Difference between revisions of "ELTSS:FHIR IG Proposal"
| Line 3: | Line 3: | ||
<div style="float: left;">[[Image:OpenHotTopic.GIF|35px| ]]</div> | <div style="float: left;">[[Image:OpenHotTopic.GIF|35px| ]]</div> | ||
<div style="background:#F0F0F0"> | <div style="background:#F0F0F0"> | ||
| − | This page documents a [[:category: | + | This page documents a [[:category:Approved FHIR IG Proposal|Approved]] [[:category:FHIR IG Proposal|FHIR IG Proposal]] |
</div> | </div> | ||
</div> | </div> | ||
[[Category:FHIR IG Proposal]] | [[Category:FHIR IG Proposal]] | ||
| − | [[Category: | + | [[Category:Approved FHIR IG Proposal]] |
Latest revision as of 21:41, 19 February 2019
Contents
- 1 HL7 FHIR Implementation Guide: Electronic Long-Term Services and Supports (eLTSS), Release 1 - US Realm
- 1.1 Owning work group name
- 1.2 Committee Approval Date:
- 1.3 Contributing or Reviewing Work Groups
- 1.4 FHIR Development Project Insight ID
- 1.5 Scope of coverage
- 1.6 IG Purpose
- 1.7 Content location
- 1.8 Proposed IG realm and code
- 1.9 Maintenance Plan
- 1.10 Short Description
- 1.11 Long Description
- 1.12 Involved parties
- 1.13 Expected implementations
- 1.14 Content sources
- 1.15 Example Scenarios
- 1.16 IG Relationships
- 1.17 Timelines
- 1.18 When IG Proposal Is Complete
- 1.19 FMG Notes
HL7 FHIR Implementation Guide: Electronic Long-Term Services and Supports (eLTSS), Release 1 - US Realm
Owning work group name
Committee Approval Date:
- CBCP Approval Date: 11/20/2018
- FMG Approval Date: TBD
Contributing or Reviewing Work Groups
The following workgroups own FHIR Resources that will be referenced in the IG:
- Patient Care
- Orders & Observations
- Financial Management Group
FHIR Development Project Insight ID
1431
Scope of coverage
- Subject: Human
- Disciplines: Long-Term Service and Supports (non-clinical) are comprised of a diverse set of assistances designed to help with general care, activities of daily living (ADLs), and instrumental activities of daily living (IADLs) like eating, toileting, dressing, cooking, driving, managing money, etc. These services are non-clinical in nature and are provided across various settings from facility-based or institutional care to community-based settings.
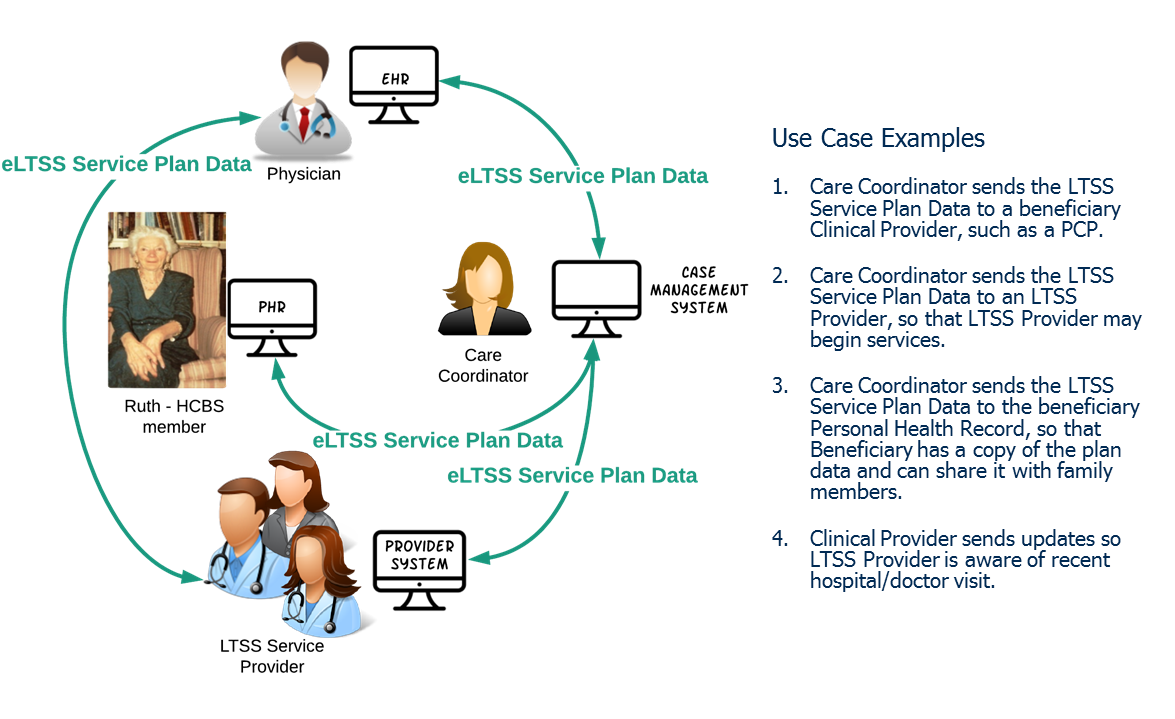
- Delivery environment: Services and supports provided in the person’s home or in a community setting are referred to as Community-Based Long-Term Services and Supports (CB-LTSS) or Home and Community-Based Services (HCBS). Systems involved in LTSS may include case management systems, PHRs, EHRs, HIEs, provider systems, Medicaid Management Information Systems (MMIS), etc.
- Locale: US Realm
Electronic Long-Term Services & Supports (eLTSS) Service Plan Project aims to enable electronic data-level interoperability and exchange of data reflected on the person-centered service plans. The ultimate goal is to leverage HIT standards and electronic information sharing to improve the delivery and coordination of community-based care provided under programs such as Medicaid Waivers. This project is the continuation of work performed under the eLTSS Initiative, a joint effort by ONC and CMS, that published an eLTSS Dataset and balloted the “HL7 Cross-Paradigm White Paper: Electronic Long-Term Services & Supports (eLTSS), Release 1” in the Sep 2018 ballot cycle. Current HL7 Standards include content to enable the creation and exchange of medically-focused care plans. This effort aims to provide guidance to access and exchange community-based service information alongside the medical interventions for a comprehensive picture of a person’s care.
The IG will use FHIR US Core R4 as a starting point and will profile the following resources as necessary to enable eLTSS Plan Creation and Exchange:
- CarePlan
- CareTeam
- Claim
- Condition
- Contract
- Coverage
- DocumentReference
- EpisodeOfCare
- Goal
- Location
- Observation
- Organization
- Patient
- Practitioner
- Questionnaire
- QuestionnaireResponse
- Related Person
- RiskAssesment
- ServiceRequest
IG Purpose
The adoption and use of Health IT and quality measurement for community-based long-term services and supports is limited. Limitations include:
- lack of uniformity in the terminology and definitions of data elements, including those important to the beneficiary, needed for assessments and service plans used across and between community-based information systems, clinical care systems and personal health record systems;
- insufficient business and/or financial incentives for service providers to acquire and use Health IT to support coordination of services;
- minimal national standards for quality measurement in LTSS outcomes;
- lack of consensus on the inter-relationships between a beneficiary’s plans across care, services and supports; and
- lack of evidence and understanding of how Health IT may benefit the beneficiary and encourage their adoption and use of Health IT.
- lack of established best practices for complying with legal security and privacy requirements when electronically exchanging data between covered clinical entities and non-clinical entities providing community-based services.
The eLTSS FHIR IG will help drive the discussion to begin to remove these limitations by providing an official compilation of all the FHIR-related artifacts and documentation needed to enable exchange of eLTSS Dataset via FHIR (e.g. eLTSS Dataset FHIR mappings, eLTSS data exchange scenarios, examples). The IG will be matured to a Standard for Trial Use (STU) and will serve to support continued testing activities and evaluation by implementers.
Content location
Additional Project Background Available Here:
Proposed IG realm and code
US/eLTSS
Maintenance Plan
The project is funded through ONC and CMS. The maintenance plan is to follow the path as the US Core FHIR IG where the initial content is developed and adopted by various pilot organizations and networks and then transition the Implementation guide to the owning work group (CBCP) for the long term.
Short Description
Provides guidance to US Realm implementers to use the FHIR for implementing access and exchange Electronic Long-Term Services & Supports (eLTSS) Dataset data elements
Long Description
This US Realm IG covers interfaces for non-clinical and clinical entities (e.g., EHR, PHR, HIE, case management systems) and provides gives guidance for implementing the Electronic Long-Term Services & Supports (eLTSS) Dataset for the collection, exchange and sharing of Home and Community Based Services (HCBS) data, clinical data and provider service plans. Guidance includes eLTSS Dataset FHIR mappings for service plan information, non-clinical and clinical data.
Involved parties
Community Based Care and Privacy (CBCP) is the primary sponsoring workgroup. A collaborative team made up of ONC and CMS contractors (SRS, Carradora, Georgia Department of Community Health (supported by Georgia Tech)) will create the IG.
Expected implementations
- CMS, ONC
Content sources
This project is the continuation of work performed under the eLTSS Initiative, a joint effort by ONC and CMS, that published an eLTSS Dataset and balloted the “HL7 Cross-Paradigm Information Sharing for Electronic Long-Term Services & Supports (eLTSS), Release 1” Informative Document in the Sep 2018 ballot cycle. A multi-state (CO, CT, GA, KY, MD, MN) consensus-based approach was used to identify and harmonize the eLTSS Dataset.
The IG will depend on US Core profiles for applicable eLTSS data.
Example Scenarios
LTSS is currently a document-oriented exchange paradigm (i.e., consumers exchange the entire service plan as a document), however during outreach stakeholders expressed an interest in the ability to exchange portions of service plan data, query specific elements, receive notifications, etc. The aim of eLTSS is to enable those exchanges and features for LTSS data.
- Use the following FHIR Resources to generate an eLTSS plan in an LTSS case management system
- Bundle, CarePlan, CareTeam, Claim, Condition, Contract, Coverage, DocumentReference, EpisodeOfCare, Goal, Location, Observation, Organization, Patient, Practitioner, Questionnaire, QuestionnaireResponse, Related Person, RiskAssesment, ServiceRequest
- Exchange eLTSS Plan from Support Planner (case management system) to Clinical and Institutional-based Provider (EHR system)
- Purpose: The clinical and institutional-based provider is informed of what service(s) the Beneficiary is eligible for and to supply additional details around the services as well as the Beneficiary to enable better delivery of services and support.
- eLTSS Data: Clinical and Institutional-based Provider may need cost information (Claim), emergency backup plan (CarePlan), full details on service quantities (ServiceRequest), etc. Important information includes contact information for a financial management worker (Practitioner).
- Exchange eLTSS Plan from Support Planner (case management system) to HCBS Provider (provider system)
- Purpose: To inform HCBS Provider of service(s) requested by Beneficiary, or are authorized for the Beneficiary, as well as to supply additional detail around those services and the Beneficiary to enable better delivery of services and supports.
- eLTSS Data: HCBS Providers need service and cost information (Units and Unit Costs, Effective Dates, etc.) (ServiceRequest, Claim), especially if there is a change (i.e., due to a re-assessment). This use case would be the vehicle to communicate these data elements to the HCBS Providers officially, even if the services (and quantity and rates) were previously negotiated. Signatures (Contract) are not required; however, the eLTSS Signature Date data elements (Contract) indicating when the plan was approved (CarePlan) could be important.
- Exchange eLTSS Plan from Support Planner (case management system) to Beneficiary (PHR)
- Purpose: The Beneficiary has a complete record of what is either proposed or to be provided to them and by whom, and potentially be imported into the Beneficiary’s PHR.
- eLTSS Data: Beneficiary will not need signatures (Contract) and may not need cost information (Claim).
- Exchange eLTSS Plan from HCBS Provider (provider system) to Clinical Provider (EHR) (vice versa)
- Purpose: The Clinical Provider is aware of the services the Beneficiary is receiving and what their goals/needs/risks are or have been. The HCBS Provider is aware of the Beneficiary's recent hospital/doctor visit and any discharge/treatment instructions to follow.
IG Relationships
Dependent on the US Core IG where applicable for eLTSS (e.g., Patient, Care Plan, Document Reference, Goal, Condition, Practitioner)
Timelines
- 2/17/2019: Submit a functionally complete IG to CBCP along with the Notice of Intent to Ballot (NIB) to CBCP.
- 3/3/2019: Submit a complete FHIR IG to HL7 for QA.
When IG Proposal Is Complete
When you have completed your proposal, please send an email to FMGcontact@HL7.org